Human Learning Systems: A Complexity Friendly Approach to Public Services


Can the @systemshuman approach reshape home care for the older people? See how @wellbeingteams have reconceived ‘good care’.
Share articleBring your whole self to work. @HelenWBTeam tells @tobyjlowehow shared leadership shaped homecare @wellbeingteams
Share article‘What does a good day look like?’ Learning together to support people live their good lives through homecare @wellbeingteams
Share articleWe put our vision for government into practice through learning partner projects that align with our values and help reimagine government so that it works for everyone.
We often hear that the UK’s health and social care system is in crisis. People deserve to be cared for properly and with dignity, we say. Yet our care system is not currently organised to enable the best possible outcomes for those who need it most. The reasons for this are varied, but one critical barrier is the rigid commissioning guidelines that are based on a ‘time and task’ model and often don’t allow for the bespoke, human care we know that families and home carers want for those in care.
Wellbeing Teams are pioneers of a self-managing teams approach to home care. Dr. Toby Lowe recently spoke to Helen Sanderson, Founder of Wellbeing Teams, to find out more about how they create outstanding care, based on their teams in Wigan and Oxford, and now Thurrock and Camden. They are the first in the UK to use self management in home care and achieved the first ‘outstanding’ rating from the CQC for a self-managed team – a rating that only 4% of home care achieve on their first inspection.
They discussed how Wellbeing Teams were early adopters of what’s become known as the Human Learning Systems approach to public service, which encourages everyone to be recognised as individuals with unique strengths and needs, and puts the relationship between carer and those they care for at the forefront of practice..
It all began when Helen decided to put into practice everything she had been learning about self-management in her consultancy work into community and home care. She saw that good care should start with empowered care workers.
“Inspired by LaLoux’s book ‘Reinventing Organisations’ and as a consultancy team, we started by moving to self-management. This meant that I gave up the position of CEO. Two years later, I went back to LaLoux’s book and re-read the case study of Buurtzorg and their principles. I wondered if we could do something like that in the UK in social care. I wanted to get ‘skin in the game’ and demonstrate self-management with a relational and community focus to support. Therefore the purpose of Wellbeing Teams became, ‘to help people to live well at home and be part of their community.’”
People deserve to be cared for properly and with dignity, we say. Yet our care system is not currently organised to enable the best possible outcomes for those who need it most.
The current commissioning system simply isn’t set up for good care. Commissioners buy blocks of time in 15-30 minute increments. Travel time may not be included in their schedules so they rush from one visit to another, and seldom have time to form relationships. Wellbeing Teams moved away from a model that is task and time-based to one focused on care relationships.
“In Wigan, our first Wellbeing Team three years ago, the majority of the outcomes and tasks were for supporting people to get up, get clean, have medication, have food, get undressed and go to bed. This would usually be three thirty-minute visits a day. This did not give us much leeway to support people to do what matters to them or build community. We were fortunate to be supported by the charity Making Space, which is how we could achieve so much more.”
Half of the 670,000 employees across the social care sector are on zero hour contracts, and underpaid and undervalued staff are unable to deliver the care and attention someone needs. The workforce is under-resourced and often unmotivated, with a 65% churn rate. By contrast, Wellbeing Teams have less than 5% churn. Part of this is that the staff are paid a salary rather than shift work, which is set at or above the living wage, but it is also because they are trusted to build relationships, learn and improve together. And so they are more likely to enjoy the work.
Good care is varied, complex, and not always easily controllable – like people. Good care for Wellbeing Teams is about supporting people to have good lives in the community. “We ask people what a good life looks like for them. It may be about getting back to a faith community, taking up knitting again or feeding birds in the garden.”
That is the conversation that every relationship begins with. Wellbeing Teams want to know what matters to the person, and ask everyone ‘What does a good week look like to you?’ The team member then discusses with the person being supported , the Wellbeing Team, family and social prescribing link workers what they can put in place to facilitate that.
“I believe people want to live at home. Communities are better when everybody is part of them, and we live better lives when we are connected to our communities,” Helen explains.

Throughout their discussion, Toby and Helen hit on exactly what the Wellbeing Teams approach is about: “learning together.” As Helen explains it, “every conversation is a process of discovery.”
“We focus on relationships and use a strengths-based approach. We talk to the people we support about their strengths, their gifts of the head, hands and heart, and explore whether there are ways that they want to both connect and contribute. We use the same questions with team members, discovering their gifts of head, hands and heart, and see where we can match them to what people we support want to do.”
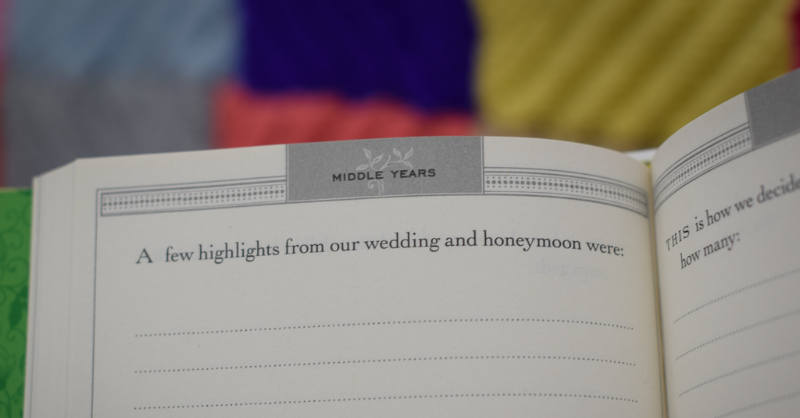
The team build one-page profiles for everyone involved. That’s the people they work with, and the team members delivering support. They create beautiful life story books so everyone can capture their stories and know that they've been really listened to.
Sometimes those conversations spark new ideas. In fact, that is crucial. Support is designed around the passions and purpose that enable people live a good life.
As Helen describes, “I was once on shift, shadowing a team member on a Sunday morning and was admiring the knitting that the wife of the person we were supporting had done. When I asked her about it, she said: ‘I really enjoy it but no one wants knitted things anymore.’
We did six visits that morning and I talked to everyone we supported about knitting, whether they had ever done it, whether they were interested in it, why people knitted these days. I asked on social media, and a local mum said that when her daughter was in the special care baby unit, there were knitted blankets around and it made it feel less clinical. This led to the ‘Knit and Natter group’ starting in a local café. We became well known and other people would join in. The group knitted blankets for the local special baby care unit. There was usually more nattering than knitting, but the group had a sense of purpose, and led to connections with new people and new friends.”
The group was about more than knitting – it was about community, connection, and purpose.

Good care starts with empowered staff. Values-based recruitment was a big part of the process. Anyone can be trained to deliver good homecare, as long as they have the values that allow for it. Wellbeing Teams won a Guardian Public Services Award in recognition of their work in this space, one of four awards in 2018 alone.
60% of Wellbeing Teams staff had not worked in health and social care before, and 80% were from outside home care. This means that team members didn’t have to “unlearn notions of professional boundaries and those kinds of things, because those are the things that really get in the way of people being together and learning together.”
Team members are encouraged to bring their whole selves to work. The system is not only about what they can give to others, but about how they can grow and develop themselves, enjoying their work, whilst also being paid fairly for it. Those one page profiles aren’t just for those people being cared for. Staff also have profile pages with their strengths, goals and areas for development included.
Wellbeing Teams work in a way that is emergent, opportunistic, and creative. As is at the heart of HLS, they embrace the opportunity to learn and discover, without being bound to a rigid way of working. Helen says that “it’s a principle to be maintained, rather than a model to be applied.”
“Continuous learning drives process and performance development. In our first year, I rewrote the Wellbeing Handbook six times because we had learned so much through failure. Difficulties showed we need to quickly learn how to do things differently.”
Progress charts are a standard part of homecare. Wellbeing Teams took a different approach, seeing what worked for each individual and what could be done next time to make it better. “We have weekly meetings to ask what is on track, and what needs to happen to keep it on track or get back on track, monthly reviews via Peakon questionnaires, as well as more formal six month meetings.”
Shared leadership is also a departure from the norm, with typical manager roles shared by the team. Support is key with peer learning and coaching from a Wellbeing Leader. Team members are asked to bring their whole self to work, and also have a summary profile which considers their “gifts of head, heart and hands.”
“As a team member your role is to support somebody to have the best life they can, at home and as part of their community, and that includes making their day and bringing your gifts and talents and your passions into play. How we work with each other will have a huge impact on how happy the people we support are, because how you show up as an individual matters.”
Continuous learning drives process and performance development. In our first year, I rewrote the Wellbeing Handbook six times because we had learned so much through failure. Difficulties showed we need to quickly learn how to do things differently.
Working with the CQC was itself a process of relationship building and learning. To enable their ‘Outstanding’ rating, the teams looked at the metrics that mattered to them, as well as those needed by CQC. Their outstanding rating demonstrated that self-managed models of care are congruent with and supported by regulatory processes.
But unfortunately they found that they were not possible within the current commissioning model. In Wigan, Wellbeing Teams saw out the end of the contract they started, and Oxford finished after the pilot. But in Thurrock things are looking promising, and Wellbeing Teams partnered with Camden Council to set up two teams supporting people in Extra Care.
The commissioner in Thurrock was braver and worked with us to develop two teams where the support was commissioned differently, and the focus was on wellbeing. Early indications show that over the last two years if you were supported by a Wellbeing Team in Thurrock, you were five times less likely to go into hospital. So as well as being excellent for the people concerned, that is also a massive saving to the health system. However, the challenge is that Wellbeing Teams is saving money for a different pot than from which it is commissioned.. These are some of the system changes that we need to see, and Thurrock is leading the way in this. This isn’t a limitation of Wellbeing Teams, but a systemic issue with the care process. We need a different commissioning model to make this happen.”
“It just shows that home care problems aren’t native to the work itself, but symptoms of how it has been conceived, commissioned, managed and evaluated. We are reconceiving the traditional scope of home care. ” she explains.
People have been trying to work to rehumanise public service for a while now. Human Learning Systems supports this by bringing about change in public management practice, which enables people to think differently about commissioning, and other aspects of the integration of health and care systems. There is much we can learn from the pioneers at Wellbeing Teams.
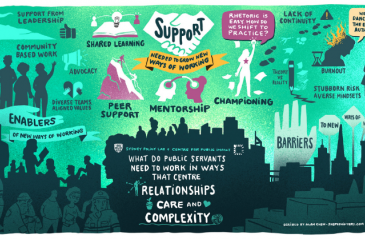
We’re exploring how Human Learning Systems can offer a complexity-friendly approach to public service delivery in line with our emerging vision for government. In this series, we highlight the stories of government changemakers who are pioneering this approach - their breakthrough moments, successes, and what they’ve learned from failure - as well as what we’re learning from them along the way.