
The UK Human Fertilisation and Embryology Authority’s "One at a Time" campaign
In-vitro fertilisation (IVF) involves collecting eggs, fertilising them with sperm in a petri dish, and then transferring them back into the womb. When more than one embryo is transferred - typically to increase the chances of a pregnancy - becoming pregnant with twins or triplets is a possibility. Such multiple pregnancies and births pose a significant health risk to women and their offspring. In 2005, IVF success rates approached those of natural conception, but over a quarter of the babies born in the UK were twins.
This prompted the UK's fertility regulator, the Human Fertilisation and Embryology Authority (HFEA), to explore what other countries had done and to promote elective single embryo transfers (eSET) in its “One at a Time” campaign. Following a consensus statement from the sector's key stakeholders, the HFEA introduced a 10 percent multiple births target in 2009 and required clinics to develop their own eSET policies. These specified that women with higher chances of conceiving should only receive a single embryo transfer. In 2016, the national multiple birth rate was at 11 percent, while success rates had continued to rise. Balancing clinical autonomy and the patient's right to choose with unambiguous targets and monitoring in the face of a public health threat is the essence of the HFEA's successful strategy.
The initiative
In 2007, the HFEA launched a national strategy to reduce the incidence of multiple births after fertility treatment by promoting elective single embryo transfer (eSET) as part of their “One at a Time” campaign. Transferring just one fertilised embryo at a time back into the womb of patients who are most likely to get pregnant reduces the risk of multiple births while maintaining overall success rates.[4]
The HFEA established One at a Time together with professional bodies, patient groups and NHS funding bodies, and obtained their commitment for the following aims by means of a consensus statement:
- Reducing multiple birth rates following IVF - thereby achieving better health of mother and child
- Maintaining live birth rates
- Maintaining the overall cost of treatment for patients
- Respecting the doctor/patient decision-making process - by not drawing the HFEA into the autonomy of clinical decisions unnecessarily.[4][6]
After a public consultation, the HFEA published new guidance for clinics in January 2009. The policy:
- Introduced multiple birth targets in a stepwise fashion, with the ultimate goal of reducing the rate to 10 percent
- Required all clinics to formulate their own strategy on how to achieve these targets
- Added multiple births as a practice area subject to inspection, aided by an alert system which notified inspectors in real time to noncompliance.[3][5]
The HFEA and its partners also launched several measures to support the initiative. The One at a Time campaign aimed to provide “clinics with the tools to change their clinical practice [by sharing best practice examples], [worked] to improve NHS funding of fertility treatment and [provided] information to patients” through a central website.[7]
Furthermore, the HFEA added a chapter on multiple births to its Code of Practice, incentivised eSET by discounting the fee it charges clinics for every treatment cycle, updated clinic data collection forms to change the way success rates were displayed, organised regular stakeholder group meetings, and set up workshops throughout the country to promote best practice. “Whilst the HFEA set the policy targets, the joint BFS/ACE guidelines published in 2008 provided guidance to fertility centres on how their clinical practice could change to meet these targets.”[3] In 2011, a special stakeholder summit reaffirmed the commitment of all campaign parties with an updated consensus statement.[8]
The challenge
Reproductive medicine has come a long way since the first “test tube baby”, Louise Brown, was born in 1978. “Bristol railway man John Brown and wife Lesley had been trying to conceive for nine years without success when they encountered Oldham-based obstetrician Dr Patrick Steptoe and his research partner, Cambridge physiologist Dr Robert Edwards, in 1977.”[1] The researchers had been working on an experimental technology called in vitro fertilisation (IVF), and later that year implanted Ms Brown with an embryo “from a petri dish rather than a test tube”.[1] Nine months later, the birth of a healthy baby girl made headlines around the world.
What was once a sensation has become the primary treatment for overcoming infertility.
While IVF birth rates have improved from 14 percent per treatment cycle in 1991 to 24 percent in 2006, this has been marred by the high rate of multiple births.[2] In 2008 it was estimated that around a quarter of IVF births were multiples, compared to just 2 percent from natural conception. It was estimated that half of all twins were born as a result of fertility treatment.[3][4]
A multiple birth, meaning the delivery of twins, triplets or more than three babies, is the single biggest health risk associated with fertility treatment, for both mother and children:
- Mothers have a higher risk of miscarriage, gestational diabetes, severe bleeding and other complications in pregnancy
- The babies are more likely to be premature and have a low birth weight
- The number of deaths within the first month of life increases from 3 deaths per 1,000 live births for singletons to 19 deaths per 1,000 live births for multiple babies
- The risk of cerebral palsy increases from 1.7 cases per 1,000 live births for singletons to 6.2 cases per 1,000 live births for twins
- There are also well-documented problems for families of twins that range from financial hardship to a higher incidence of maternal depression and marital problems.[4]
This means that the birth of a healthy singleton child, born at full term, is the safest outcome of fertility treatment for both mother and child.[5] The primary cause of the increased rate of multiple births is the practice of transferring multiple embryos during the same IVF cycle.
Despite this, both fertility clinics and their patients accepted the risks associated with multiple births, sometimes favouring twins. For clinics, there was an incentive to transfer two embryos in the same treatment cycle, which might boost the success rates that most patients look to when choosing a clinic. Patients themselves often preferred to have twins, given their years of trying unsuccessfully to have children. This was because they often did not want, or did not have the financial means, to go through another costly and often stressful treatment cycle. The problem was exacerbated by the limited and sporadic public IVF funding provided by the National Health Service (NHS). Even though over two-thirds of patients were informed about the risks of multiple births, 91 percent still favoured multiple embryo transfers.[4]
As a result, in 2005 the Human Fertilisation and Embryology Authority (HFEA), the UK government's independent regulator of fertility clinics, commissioned an expert group to examine multiple births after IVF and the possible solutions. The group's 2006 report “provided irrefutable evidence that the extraordinary rise in the prevalence of twin births in the UK is in the main due to fertility treatment, particularly IVF”.[6]
The public impact
Rigorous analysis of the problem, strong stakeholder engagement, and clearly measurable targets made the HFEA's strategy for reducing multiple births a successful public health initiative. One at a Time achieved a significant reduction in multiple births - from 26 percent in 2005 to 11 percent in 2016 - while IVF success rates per embryo transferred increased by 7 percentage points to 21 percent over the same period. This was due to laboratory advances that meant embryos could be cultured to the blastocyst stage. IVF outcomes remained stable: in 2016, 26 percent of treatment cycles resulted in a birth, up by 3 percent from 2005.[2]
Although the 10 percent target had been narrowly missed, a clinic-level analysis revealed that this was probably due to outliers, because the vast majority of fertility centres were fully compliant. Out of 119 clinics, 86 percent met the target of having no more than 10 percent multiple births in FY 2016/17. Of the remaining 14 percent, half were monitored closely because they were at risk of failing to meet the target and the other half were statistically above the target. There were 14 noncompliant clinics in this category in 2015/16, but this fell to 6 clinics in 2016/17.[9]
Implementation at clinic level meant that doctors retained their professional autonomy by recommending eSET primarily to younger and therefore more fertile patients. This lasting change in clinical practice was further reinforced by professional societies updating their guidelines, as the HFEA ensured their continued investment in the success of the policy. In 2008, the Association of Clinical Embryologists and the British Fertility Society jointly published best practice guidelines on eSET, “intended to assist ART [Assisted Reproductive Technologies] clinics in the implementation of an effective eSET policy”. These were updated in 2015.[10]
However, it is not possible to estimate the policy's impact on treatment costs for patients. The HFEA does not regulate or monitor the price for IVF cycles, and the wide disparity of services included in standard packages makes it difficult to compare price lists, which are further split between NHS and self-funding patients. Access to fertility treatment continues to be a challenge for the sector, as cost pressures on the NHS meant that fewer and fewer Clinical Commissioning Groups offer three treatment cycles, the number recommended by the UK's National Institute for Health and Care Excellence (NICE).[11]
However, minimising multiple births reduces the likelihood of incurring antenatal and postnatal care costs or the potentially lifelong costs of medical and social support, as well as relieving the pressure on health and social care services. In addition to international evidence, a major 2018 study funded by the HFEA and its partners found that the average cost of a twin birth to the NHS in 2018 was GBP13,959 - compared to GBP4,892 for an average singleton. The report went on to say that “for every 10 percent reduction in the current rate of multiple births, GBP15 million could be saved by the NHS”,[12] an indication of the opportunities for financial improvements that remain.
In its business plan for 2019/20,the HFEA has set out to “continue to communicate about the importance of reducing multiple births to ensure safe outcomes for patients and relaunch the multiple births stakeholder group”.[13] Identifying how to help clinics make further progress will be key to maintaining the momentum of its eSET strategy.
Written by Stevan Ćirković
This case study was written in Stevan's private capacity
Stakeholder engagement
Before the launch of One at a Time and the implementation of multiple birth targets for clinics, the HFEA engaged extensively with stakeholders, including providers of fertility treatment (clinicians, embryologists, and counsellors), patients, and the public. In January 2007, the HFEA convened a wide range of professional societies and patients' organisations to develop a common position on the multiple births problem. As a result, a consensus statement was published in April of the same year with a total of 20 signatories, including all the sector's main players such as the British Fertility Society and Fertility Network UK.[6]
The consensus statement followed a meeting of stakeholders convened by the HFEA, which took place in London on 23 January 2007. In the statement, the stakeholders committed to a single solution: “the direct link between the number of embryos transferred to the uterus during IVF treatment and the chance of twin pregnancy is beyond dispute... The only way to reduce multiple birth rates after IVF is to transfer only one embryo to those women at most risk of having twins. eSET and the freezing of any additional suitable embryos should be standard practice in good prognosis IVF patients.”[6]
The document also ascribed various roles to the different organisations in achieving the common goal. For example, fertility clinics were to change their practices and inform patients of the benefits of eSET, professional societies were to develop new treatment guidelines, and the HFEA was to develop regulatory measures, as the signatories had agreed that “a degree of prescription is likely to be required to facilitate change in practice and attitudes”.[6]
Importantly, the consensus statement proposed various options to achieve this end, and the eventual 10 percent target was only decided after the HFEA had completed a public consultation in July 2007.[14] The elements of the consultation were: a written questionnaire, three patient focus groups, and separate consultation meetings with practitioners and patients. In total, 907 participants were consulted.[15] However, of the written responses, a mere 3 percent supported the HFEA setting a maximum rate, with 83 percent of individual patients and 55 percent of practitioners preferring eSET to remain at the discretion of the patient and their doctor.[15] The HFEA was criticised by the patients' organisation TAMBA for ignoring these views.
Political commitment
In creating and enforcing its multiple births policy, the HFEA used its political weight and legal powers as the UK government's independent regulator of fertility services. As such, it is set up as an “executive non-departmental public body” with affiliation to the Department of Health. It operates “at arm's length” from the minister and is overseen by a board, thereby ensuring both political neutrality and public scrutiny, with its remit being defined in the Human Fertilisation and Embryology Acts of 1990 and 2008.[16]
In engaging the public, the then HFEA chairman Shirley Harrison made it clear that the risks arising from multiple births were largely avoidable, demonstrating her willingness to spend political capital in spreading the message. "Doing nothing is not an option. The latest figures show 126 IVF babies die each year because they have been born as twins not single babies. We can't let that continue," she said during the public consultation in 2007.[17] This statement was made at a time in when “many patients [saw] twins as the ideal outcome of IVF” and some fertility doctors warned the HFEA against an indiscriminate eSET policy.[18]
Public confidence
The HFEA commanded relatively stable public support in its vital role in regulating the sector, giving it the necessary legitimacy to balance competing interests in tackling the multiple births problem. The HFEA operates in a field of medicine that continues to spark public controversy, because scientific advances in embryology and fertility treatment raise complex ethical, legal and social questions. Social egg freezing, preimplantation genetic diagnosis, and mitochondrial donation (“three-person babies”) are just a few examples of topics that have attracted heated debate.[19]
From a regulatory perspective, it is relevant that the field of reproductive medicine is characterised by very strong individual and personal interests that sometimes stand in opposition to the public interest and scientific evidence. For example, a 2007 study showed that women undergoing IVF preferred a risky pregnancy to no pregnancy, with little appreciation of the dangers of multiple births.[20] Similarly, clinics sometimes take issue with regulations and standards set by the HFEA that limit or modify ways in which they can take on new patients and offer treatments while trying to maximise success rates and be accountable to the watchdog for their practices.[21] These conflicts of interest explain why only 3 percent of respondents in the 2007 public consultation supported the 10 percent target for multiple births, although few in the sector disputed the seriousness of the problem.[15]
It is therefore worth looking at the support for the HFEA's role as a regulator. In the 1980s, only a few years after Louise Brown's birth, the need for an independent oversight body became clear. The report of a government inquiry into the emerging field conducted between 1982 and 1984 concluded that “people generally want some principles or other to govern the development and use of the new techniques. There must be some barriers that are not crossed, some limits fixed beyond which people must not be allowed to go.”[22]
The HFEA was eventually set up in August 1991 under the provisions of the Human Fertilisation and Embryology Act 1990. Before the revision of the Act in 2008, the public debate focused on contentious issues of the day such as the rights of same-sex couples, but there was continued support for the role of the HFEA.[23] When the abolition of the HFEA was seriously considered in 2010 and 2011 to save money and streamline public services, doctors, scientists and other stakeholders vehemently defended its continued existence and the government ultimately changed its mind.[24][25] All of this serves as solid evidence of citizens' confidence that the HFEA would act in their best interest.
Clarity of objectives
In its 2006 report, the Expert Group on Multiple Births after IVF agreed a number of objectives for any policy response to the multiple births problem:
- “The number of multiple births following IVF is reduced, thereby reducing the morbidity and mortality of mothers and babies and the pressure on NHS children's services
- “The overall cost of treatment for patients does not increase significantly if more cycles are needed
- “Live birth rates per stimulation cycle started are maintained as far as possible;
- “Other aspects of patient care are not compromised
- “The doctor/patient decision-making process is respected
- “The HFEA is not drawn unnecessarily into the autonomy of clinical decisions
- “Clinics develop better embryo selection practices.”[4]
Following the 2007 consensus statement and public consultation, the HFEA moved to implement a 10 percent target to promote eSET and minimise the risk of multiple births from IVF treatment. Since 2009, all clinics must have their own eSET strategy, which defines how they intend to lower their multiple birth rate to within the maximum set by the HFEA. From 2009 to 2012, the HFEA lowered the maximum multiple birth rate each year stepwise from 24 percent to the ultimate target of 10 percent.[5]
This stepwise and deliberative approach of first convening an expert group facilitated stakeholder involvement in the formulation of objectives. In late 2007, the HFEA's members committed to clear and measurable targets, even though they were unpopular with IVF patients in particular (see also Stakeholder Engagement and Political Commitment).[15]
Strength of evidence
To understand high multiple birth rates in the UK and their contributory factors, the HFEA commissioned an expert panel in 2005. The experts recommended an eSET policy based on a comparative analysis of policies in other countries, the impact of these strategies on the birth of twins and triplets, and how these solutions could be transferred to the UK.[26]
Reviewing international policies to reduce multiple births after assisted conception in a country-by-country table, the report concluded that “other countries such as Belgium, Australia and Sweden had shown that low multiple rates could be achieved by eSET in those women most at risk”.[3]
By comparing interventions, their impact, and the overall policy environment, the expert group also identified a key difference between the UK and the countries that had pioneered eSET: “generally patients [in those countries] have better access to publicly funded IVF treatments, which directly influences patients' attitudes to eSET”.[4] The call to expand access to national funding for IVF was hence included in the report and the 2007 consensus statement.[4][6] By commissioning a pool of experts, the HFEA implemented a solution that was supported by clear evidence of reducing multiple birth rates in other countries.
Feasibility
By promoting eSET, which had already successfully reduced the number of multiple births in several other countries, the HFEA ran a low risk of encountering challenges to the feasibility of its campaign. Relying on the existing inspection system and on clinics setting their own policies to achieve the 10 percent target, the human resource implications were also negligible.
The 2006 expert report identified the potential “obstacles to progress”,[4] which included:
- A disproportionate rise in the cost of IVF to patients
- “The failure to implement fully the NICE guideline on fertility treatments in England and Wales...
- “The consequent lack and inconsistency of NHS-funded IVF in the whole of the UK.”[4]
In particular, neither the HFEA nor any of members of the stakeholder group had exclusive control over the cost and public funding of IVF. The HFEA does not regulate cost and funding for fertility treatment in England, as it was decided locally by Primary Care Trusts before 2013, and since then by Clinical Commissioning Groups. There are still other systems in place for Scotland, Wales, and Northern Ireland.[27] As a result of their limited means of addressing the problem directly, the HFEA has failed to increase the level and scope of public funding. This is the sole objective of its One at a Time campaign that the HFEA has not delivered. However, this objective has proved to be less relevant than expected in achieving the multiple birth rate target.
In 2011, the HFEA attempted to reinforce its eSET policy by introducing “a condition of a fertility clinic's treatment and storage licence not to exceed the multiple birth rate target”, but it was successfully challenged in the courts by two clinics.[28] Licence conditions are the most powerful instruments with which the HFEA can regulate, because noncompliance can lead to a clinic's licence being revoked, effectively putting it out of business. After the UK High Court ruled in 2013 that this was unfair to the claimants, the HFEA decided to withdraw the instrument for all clinics. The HFEA chair, Lisa Jardine, clarified the point that the verdict did not affect the eSET policy: “the policy stands and we will still expect clinics to bring the multiple birth rate down to 10 percent - in the interests of IVF mothers and their babies”.[29]
Management
The HFEA relied on clinic-level management for the implementation of its One at a Time campaign, requiring each clinic to have its own strategy in place. Since 2009, progress against national targets and the clinics' own policies have also been monitored and inspected every two years by the HFEA.
As part of its One at a Time commitments, clinics are required to have a documented strategy to minimise multiple births, which must set out:
- How the clinic aims to reduce the multiple birth rate and stay within annual limits
- The criteria under which it would recommend eSET to a patient.
Each clinic must also conduct regular audits that assess progress in reducing its multiple birth rate and help evaluate the effectiveness of its strategy. If more than one embryo is transferred to a patient who fulfils the eSET criteria, this must be recorded in a central log. These audits and logs are then subject to review by an HFEA inspector.[30]
By issuing a general directive in 2009, multiple births became one of the areas of practice against which clinics are assessed by the HFEA. Before it grants a new licence or renews an existing one, the HFEA carries out an inspection to check whether clinics are making the improvements previously asked for and to monitor their overall progress. Its inspectors also collect feedback from patients, both online and onsite.[21] Often, inspectors have a clinical background which allows them to give advice on how other clinics have successfully minimised multiple births. A real-time reporting tool on multiple births was introduced in 2011, enabling inspectors to approach clinics that had a high probability of noncompliance and to work closely with them to comply (see Measurement).
Measurement
Fertility clinics are required to report any patient they have accepted for treatment, as well as the subsequent outcomes of the treatment, to the HFEA Register, which allows the regulator to monitor the policy outcomes in a consistent manner. Based on this data, the Register team collates success rates and multiple birth rates for each clinic at least once a year. As recommended by the expert group report, the HFEA changed its clinic data forms in October 2007, so that success rates could be displayed as “per embryo transferred” as opposed to “per cycle”. Clinics started using the new data collection forms in 2008, and they included the requirement to specify any use of eSET.[5] This made it possible to attribute the decrease in multiple births directly to the use of eSET, which was mostly in patients below the age of 37.
In 2011, the HFEA published pregnancy data for the first time and also introduced a risk assessment tool for multiple births. The main function of the tool is to “constantly and proactively monitor clinics' multiple pregnancy rates. If it becomes likely that a clinic will not meet the target, the tool will notify an HFEA inspector, who will make contact with the clinic to discuss the issue.”[5]
Alignment
Keeping stakeholders aligned throughout the implementation of One at a Time was a priority for the HFEA. Since 2007, the multiple births stakeholder group has been convened by the fertility watchdog two to four times a year to discuss the progress that has been made and any obstacles to achieving the 10 percent target. It consists of a core group of professional societies, patients' organisations, and government executives.[31] Furthermore, in 2011, two years after the official requirements for clinics were introduced, the stakeholder group updated the consensus statement of 2007 to reflect old and new challenges as well as to reaffirm a shared commitment to the eSET policy.[3]
The 2011 update reaffirmed a vital principle that has enabled a change of clinical practice without sacrificing IVF's positive impact on birth outcomes. “Each patient should be treated as an individual. Patients most likely to become pregnant, and therefore also most at risk of a multiple pregnancy, should have eSET. eSET is not appropriate for all patients. Important prognostic indicators include female age and available embryo quality.”[3]
Any treatment centres that had developed “blanket” eSET policies had to revise them. By rejecting more prescriptive options after the 2007 public consultation, the HFEA largely removed conflicting incentives between stakeholders in the fertility sector. Patients had the greatest likelihood of having a baby, while clinics did not have to fear a competitive disadvantage. Between 2008 and 2016, success rates remained stable at about 26 percent per cycle started.[9]
Bibliography
[2] Fertility treatment 2014-2016 - trends and figures (Datasheet), HFEA, 2017, https://www.hfea.gov.uk/media/2581/underlying-data-fertility-trends-tables-v2.xlsx, accessed on 1 October 2018
[3] Multiple births: An update, Rachel Cutting, Jane Denton and Anthony Rutherford, 29 August 2011, Human Fertility, https://www.tandfonline.com/doi/full/10.3109/14647273.2011.608290, accessed on 1 October 2018
[12] Joint statement on the NGA multiple pregnancy report, Multiple Births Foundation, British Fertility Society, HFEA, Fertility Network UK and the Royal College of Obstetricians and Gynaecologists, 13 September 2018, HFEA, https://www.hfea.gov.uk/about-us/news-and-press-releases/2018-news-and-press-releases/joint-statement-on-the-nga-multiple-pregnancy-report/, accessed on 1 October 2018
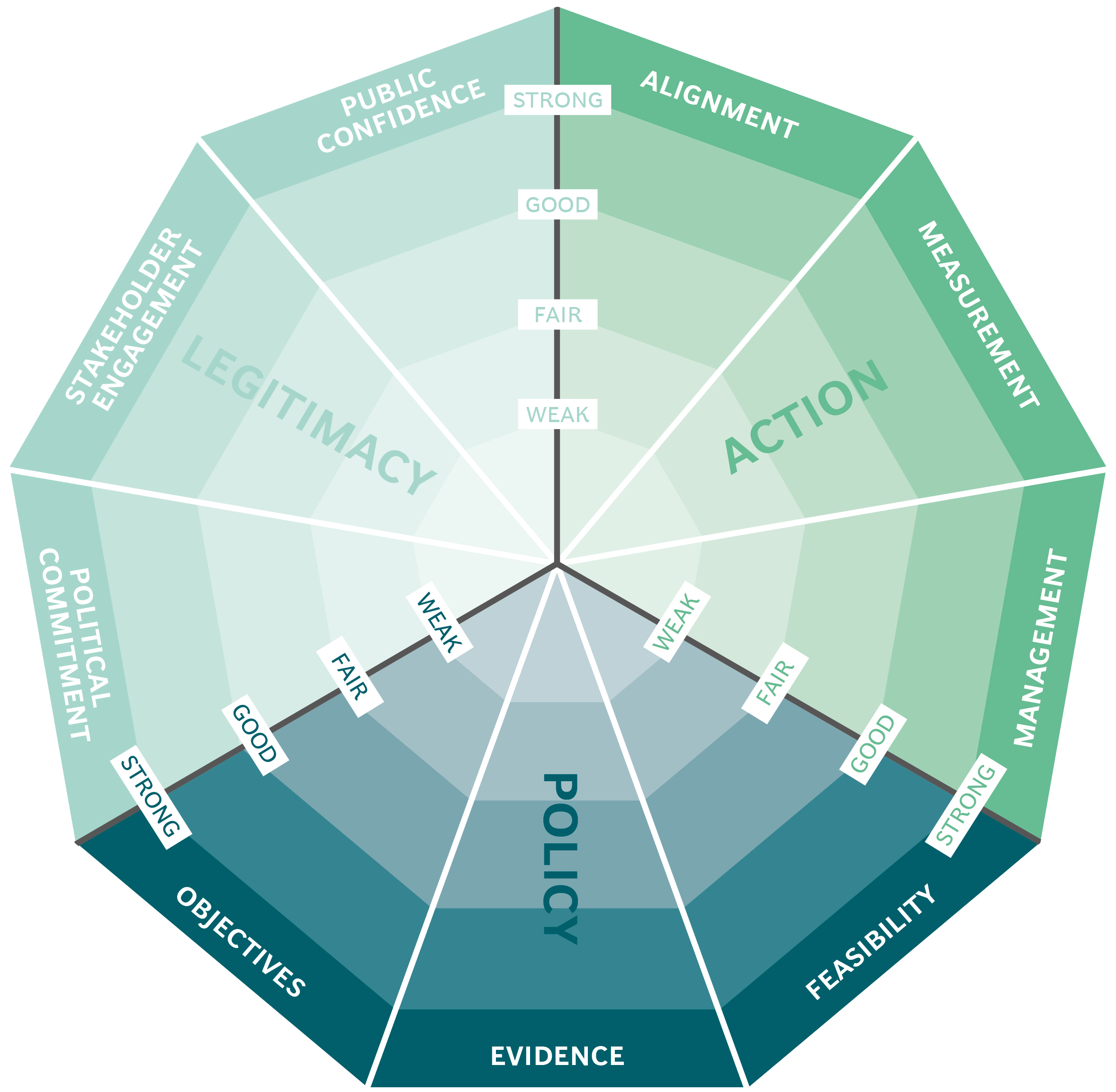
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
