
Reform 107: Belgium’s transition to a community-based approach to mental healthcare
The initiative
In January 2005, the WHO presented its Mental Health Declaration for Europe, which promoted a shift from hospital-based to community-based mental healthcare, a process known as “deinstitutionalisation”.[8] Along with several other European countries, Belgium has since made important steps towards a complete deinstitutionalisation of mental healthcare delivery. The country's mental health policymakers stimulated changes in the sector, through successive waves of pilot projects supporting the development of integrated care networks that deliver mobile and community mental healthcare. The first wave of pilot studies, which began in 2002, emphasised the development of local mobile teams providing psychiatric care. From 2005 the second wave of pilot studies focused on the development of therapeutic consultation within mental healthcare networks and circuits.[2]
In 2010, the Belgian federal government took this policy a stage further by implementing Reform 107, legislation to apply a community-based model to the Belgian mental healthcare sector. This structural reform of mental healthcare delivery aimed to:
- Strengthen the community-based supply of care
- Improve the integration of care providers
- Improve the social rehabilitation of users
- Reduce the number of psychiatric hospital admissions.[1]
The reform is based on the establishment of networks of services that are intended to supply comprehensive care circuits to specific target groups of users, while implementing collaborative procedures to supply integrated care across the different welfare sectors.[7] Every local geographic region has a youth circuit and an adult circuit within each linguistic group, with a total of six different groups of users across Belgium. Network services include home treatment teams, early interventions, and diversity of service provision; they are provided in large part through the reorganisation of care delivery within existing services. A care circuit is the whole provision of care programmes and care services for a specific target group of psychiatric patients.
At the core of the policy are five care functions that define the type of care that has to be delivered in partnerships between community- and hospital-based services:
- Prevention and early detection of mental health conditions
- Outreach, which is delivered by new, specialised services
- Recovery and social rehabilitation of users
- Intensive residential treatment for acute cases
- Specific housing and long-term care facilities where no other solution is applicable.[1]
The prevention and detection of mental health conditions requires primary mental healthcare services to collaborate with GPs and community mental health teams to promote awareness of mental health and identify early signs of mental health conditions. The outreach network consists of two ambulatory teams, a crisis home treatment team and assertive outreach team, which offer intensive treatment for acute and chronic mental health conditions. The recovery and social rehabilitation function engages with local services such as community centres, sports clubs, and employment agencies to encourage greater community involvement and social inclusion. Intensive residential treatment is undertaken at psychiatric hospitals in acute cases. Long-term residential facilities are provided to those experiencing mental health conditions where other solutions are not considered to be feasible.[7]
The challenge
The challenge for Belgium's government was to reform its mental healthcare system to address more effectively the needs of people experiencing challenges to their mental health. During engagements with institutions such as the WHO, Belgian ministers had realised that the organisational structure of its mental health system, which was based on hospital treatment, was in need of reform.[2] Belgium has traditionally relied on institutional psychiatric care to treat patients experiencing challenges to their mental health. In 2008, Belgium had 152 psychiatric beds for 100,000 inhabitants - the second-highest number in Europe, according to the WHO's Report on Policies and Practices for Mental Health in Europe.[3] In 2015, the numbers were relatively unchanged: “with more than 150 psychiatric hospital beds per 100,000 inhabitants, Belgium ranked itself top three in the world. It has 68 psychiatric hospitals for a population of 11.3 million inhabitants”.[4][5]
Under this structure, the mental healthcare system was unable to promote the wellbeing and social inclusion of people with mental health problems.[2] Mental illnesses have been the primary cause of missed days at work in Belgium: “approximately 25 percent of the Belgian population were experiencing some sort of psychological distress”,[6] and 27 percent of people took long-term sick leave (over 15 days) due to challenges with mental health.[5] The lifetime prevalence of at least one mental health challenge is approximately 30 percent.[5] Suicide rates (18.3 per 100,000 population) appear to be considerably higher in Belgium than in other European countries.[4][5]
The mental healthcare system has experienced a high level of fragmentation due to policy and fiscal decentralisation, funding disparities, care specialties and professions, and interagency divisions.[1] Fragmentation is a key issue for the most vulnerable patients, because they have more substantial and complex needs for medical, psychiatric and social care. Belgium is comprised of three major linguistic communities - Flemish-, French- and German-speaking - which has necessitated many special policy arrangements and reforms in its healthcare system. This has resulted in a complex distribution of policy competencies between the federal state and the federated entities.[7]
The public impact
The purpose of Reform 107 was to enable people experiencing mental health challenges to receive treatment in their home environments and social communities rather than in mental hospitals, reducing the number of psychiatric hospital beds. It improved care integration, social rehabilitation, service users' recovery and wellbeing, and their carers' quality of life.[9]
The Belgian health authorities gradually established multidisciplinary outreach teams and crisis teams in most Belgian regions. The new outreach teams are composed of hospital-based staff and liaise with healthcare practitioners and organisations at the primary care level. These teams sought to be highly central, connecting the community services that are involved in early intervention and rehabilitation with the residential services involved in intensive treatment and long-term housing facilities.[7] The teams serve all persons eligible for an acute psychiatric admission, and care for and treat selected subgroups of psychiatric patients with severe and long-term needs.[10] The crisis teams are designed to tackle short-term acute issues over a few days to weeks.
The treatment and care provided by these teams have been shown to prevent long-term hospitalisation. According to the WHO, the reform has significantly reduced the number of psychiatric hospital beds in favour of outreach services for people with mental health conditions.[9] The important changes in attitude within the mental health sector - combined with new, more local facilities in the community - have also been associated with a significant reduction in the duration of hospital admissions. Furthermore, the accessibility of specialised care benefited from this intersectoral collaboration.[9] “In 2017, 22 operational networks were established. Approximately 59 mobile teams are currently active (24 mobile crisis teams and 35 mobile teams for chronic mental health problems). The implementation of the teams has resulted in the reduction of 1,230 long-term psychiatric beds. During 2016, the teams followed more than 13,000 patients, and the treatment and care provided by these teams have been shown to prevent long-term hospitalisation.”[9]
In the Leuven region, for example, which has a population of 600,000, a crisis team and 5 outreach teams totalling 45 workers were created to treat people experiencing severe challenges with their mental health. These teams are comprised of hospital-based staff such as nurses, GPs, psychologists and psychiatrists. After 5 years, the number of hospital stays in that region had fallen by 20 percent.[11]
Stakeholder engagement
The development of Reform 107 entailed constant meetings and negotiations where different stakeholders came together to advocate for competing strategies designed to influence policy change. These meetings included policy meetings between government representatives and national and international experts; local meetings between frontline mental health practitioners and strategic meetings between managers of local mental healthcare institutions and community services.[1] This process pushed the development of a new institutional model and brought the competing parties together.
The responsibility for mental healthcare in Belgium is shared between several government bodies, clinicians, and the representatives of users' and carers' associations. For many of those stakeholders, the main purpose of the policy has been to support a balanced collaboration between the hospital sector and the community-based sector, not a complete transformation of residential care into community care.[7] The federal government and the three linguistic communities all play a significant role in the provision of mental health services. The important external stakeholders include network coordinators, service representatives, and the national and regional policymakers involved in the reform process; the internal stakeholders include clinicians, health service managers, and the users' and carers' representatives.
In 2002, all the ministers responsible for public health signed a joint declaration to provide acute and chronic mental healthcare through collaborative care networks and care circuits in geographically defined areas for three target groups - children and adolescents, working-age adults, and the elderly. This was an important step in the reform, making care more demand-oriented in that it addressed the genuine needs of people with mental health problems. Starting with the adult group, the aim is to broaden and deepen the reform over the next years to cover all regions and target groups.[9]
Within the psychiatric field, there has been some division regarding the community-based reforms. An alliance between psychiatric hospitals, psychiatrists' professional bodies, federal agencies such as the National Institute for Health and Disability Insurance, and advisory bodies such as the National Council for Hospital Facilities has favoured the autonomy of the medical profession and the self-determination of psychiatric institutions. This autonomy conflicts with the underlying principles of community psychiatry, which occurs within pre-defined circuits of care and is often initiated through referrals from care providers within the circuit.
However, there is another group, the reformist coalition, which has strongly supported the growth of community psychiatry. It consists of not-for-profit associations such as the Belgian Mental Health League, psychiatrists trained in community treatment, and progressive Belgian public health ministers, who are involved in international organisations such as the WHO. The reformist coalition's weak organisational integration is compensated for by the fact that its members share common values and knowledge.[2]
Political commitment
In Belgium, from the early 1970s onwards, several reforms have been directed at deinstitutionalisation and improving the integration of residential and community care. However, mental healthcare reforms take their time to show effect. Due to the resistance of different types of services to these reforms, the result had been an increase in sector specialisation, differentiation and segmentation - a common problem in the mental healthcare sectors of industrialised countries.
Initiatives by institutions such as the EU and the WHO have sought to address this problem. “Over the last 20 years, significant efforts have been made across Europe to encourage national and international political leaders to focus more attention on community-based mental healthcare and the social inclusion of people with severe mental disorders.”[12]
The growing acceptance of this community-based model has translated into a strong political commitment in Belgium to reforming the country's mental health services. In September 2009, the Inter-Ministerial Conference for Health decided to implement reforms, with the launch of Reform 107 by seven Belgian federal and regional public health ministers taking place in 2010.[13]
Public confidence
Public confidence in the reform was mixed due to initial scepticism about its feasibility, which was later resolved through several information campaigns.
People with mental health conditions and their families value the opportunity to choose their own treatment options and generally prefer being treated and cared for in their home environment. The new model is based on improving health and social outcomes and preventing or reducing hospital stays. This is a welcome result of the mental health reform in Belgium.[10] The government has also operated several educational initiatives to inform the general public about the reform. One programme has provided information on “the causes and consequences of mental illness”, using evening lectures, tours by mental health services personnel, and introductions to group therapy, music therapy and sports therapy.[9]
This has not always been the case. When the reform was outlined in a blueprint document that was presented to the general public in 2010, the policy guide for local actors raised many questions regarding the practicalities of restructuring the mental healthcare sector. Local actors were still focused on previous pilot projects and were not well informed about the proposed policy. Moreover, they felt uneasy with key aspects of the new mental healthcare model, particularly given that evaluation of the pilot projects had not yet been completed.[2]
Clarity of objectives
The blueprint document, Guide vers de meilleurs soins de santé mentale par la réalisation de circuits et de réseaux de soins [Guide towards better mental healthcare by implementing care circuits and networks],[14] clearly states the five general goals of the reform, which were to:
- Transform a supply-driven, mostly residential mental health service into a more diversified demand-driven mental healthcare provision, shifting mental healthcare delivery from large-scale psychiatric hospitals to smaller, alternative community services that are closer to the patient's own environment
- Reintegrate psychiatric patients into society through recovery and rehabilitation
- Establish collaborative procedures for the supply of integrated care across the different welfare sectors to create a more demand-led system
- Reduce the number and length of stays in psychiatric hospitals, saving them for acute cases only[7]
- Consolidate existing innovative community-based projects, tailoring them to patients' needs in order to address the existing fragmentation of the healthcare system[1]
The clear nature of these objectives and their consistent application has been a strength of the reform process. This was achieved through the policymaking processes related to the development of Reform 107 and its subsequent evolution. While this process involved actors with differing visions, reformist actors were able to take a leadership role and implement this reform according to the broad goals outlined in the blueprint document.[2]
Strength of evidence
Evidence of the effectiveness of a community-based care system was not gathered from the policy examples of other countries, but rather from national and local pilot projects designed to adapt the new mental healthcare model to existing circumstances.
This approach insisted on the strategic role played by the “project promoter” - a psychiatric hospital engaged in freezing a percentage of psychiatric beds to make the necessary budget available for the local community-based project - and the “network coordinator”, who is responsible for setting up five “committees of function” and a “strategic committee”. These committees are composed of mental health professionals who represent various kinds of existing psychiatric and other mental health institutions. They are responsible for the strategic planning of the local project's development. There were a number of training programmes for mental health professionals involved in the reform, including immersion courses in partner countries such as France, Switzerland and the UK.[2]
Participating hospitals were asked to submit project proposals for service networks with community-based services. Each network project was free to include any type of community partner and was requested to:
- Include its own coordination and governance processes
- Organise several circuits of comprehensive care to cover the mental healthcare needs of the entire population of a specific area. These circuits implemented new care functions and specialised services.[7]
Feasibility
The mental health reform was made possible by reallocating funds from long-term psychiatric beds to support collaboration between outpatient services and the community.[8] The funds necessary for this were provided out of the hospital budget, but the government did not specify how the different services were to collaborate.
Even though community-centred approaches to mental healthcare seem to result in fewer long-term hospitalised patients, they have not always resulted in the improvements expected in terms of symptoms and the rehabilitation into society of psychiatric patients. Several researchers, Lorant et al. 2014 for instance, have found that this is due to a lack of continuity and integration of care in such community-based models. The continuity of care is prevented in circumstances where the treatment is determined by individual choice rather than through the recommendation of the care team within the circuit. There also exists a fundamental contradiction between the need for centrality, or coordination through a central case manager, and the need for density, or a high number of care pathways to meet the needs of each individual user.[7]
In terms of practical feasibility, the policy blueprint document did not specify how the services involved in the care functions of the different networks were supposed to collaborate. It is very likely that most services will be involved in different care functions at the same time: for example, most community services will carry out preventive care as well as home treatments and rehabilitation care. Furthermore, the document does not specify in detail how the new mobile teams, the rehabilitation teams, the intensification of residential treatment units, and the consolidation of the previous community service pilot projects are supposed to be implemented and integrated.[1]
Additionally, care networks which are supposed to be embedded in a local context “vary greatly in terms of size and service types, density of network ties, and the centrality of key services. Whether one particular network structure is most suited to reach the multiple reform aims simultaneously remains unclear.”[8]
Management
While the lack of centralised coordination has led to inconsistent implementation of the model, there was strong local governance in the management and evaluation of care networks. The governance model to manage a more demand-led mental healthcare system is based on decentralised leadership, while the service networks are free to include any type of partner within a chosen geographical area.[8]
As regards coordination, the networks of services are governed by a strategic committee made up of representatives from all the main health agencies. Each strategic committee includes a network coordinator whose task is to facilitate contacts between all the network's member agencies and the organisation of care delivery. The coordinator's tasks are organisational rather than clinical. The coordinator has no power over funding matters and cannot influence funding decisions. All internal procedures and clinical interventions are designed for a self-evaluation approach, consistent with a shared governance model.[7]
By reallocating funds from institutional care, the reform aimed to reduce the high number of psychiatric hospital beds in favour of new mobile treatment teams. The teams are composed of hospital-based staff and are financed from the hospital budget but operate throughout the local community. The teams actively liaise with healthcare practitioners and organisations at the primary care level, and the service is free of charge for patients. Shared care protocols between the mobile teams, primary care practitioners, and hospitals are applied.
The more locally-oriented care networks are grouped into two multidisciplinary teams: crisis teams and outreach teams. Multidisciplinary crisis teams provide crisis resolution for people with acute or “sub-acute” psychological problems, through short-term home treatment and the strengthening of social networks. Working closely with primary care workers and social services, the crisis teams prevent or shorten psychiatric admissions through practical support, medication, and family therapy.
Outreach teams provide recovery-oriented care in the home environment for people with long-term severe mental health conditions, who are often difficult to reach. These generalist multidisciplinary teams support social inclusion, focusing on employment and accommodation. The teams offer care and treatment in a coordinated and integrated manner, focusing on continuity of care and working closely with primary healthcare workers and medical specialists. They use detailed, individual care plans developed in consultation with people with mental health conditions and their social context, i.e. their family and carers. These plans include warning signs of relapse and crisis plans, and they clearly describe everyone's tasks and responsibilities. Within their own environment, psychiatric patients and those closely involved with them are supported by their assigned team to participate actively in their treatment.[10]
Measurement
Due to the fragmentation of responsibilities within the Belgian healthcare sector, there is no data collection operation covering the entire mental healthcare system. In particular, the absence of unique patient identifiers makes it impossible to follow and track patients throughout the mental healthcare sector, especially once they receive outpatient care. Therefore, it remains difficult to measure Reform 107's performance and impact.
However, the Ministry of Health in collaboration with the Belgian Healthcare Knowledge Centre defined 11 indicators to facilitate the assessment of Belgian mental healthcare practices. These metrics include tangible statistics on suicide rates and the number of hospitalisation days in a psychiatric unit, as well as measures related to accessibility, quality and continuity of care. In collaboration with the federal public service, the Ministry of Health publishes an annual health system performance assessment that evaluates the changes in the mental health sector.[15]
It is unclear how the performance of local circuits is measured. The development of care network and care services has required both a “project promoter”, a psychiatric hospital that will freeze the use of psychiatric beds to develop a budget for the service, and a “network coordinator”, that establishes the committees responsible for the project's strategic development.[2] It is likely that any measurement of local networks and services would relate to the performance of local circuits within their budget constraint.
Alignment
A group of researchers set up a study to see if the Reform 107's main stakeholders endorsed its different objectives and how well the policy's goals have been translated into stakeholders' priorities.[1] The study indicates some disagreement between stakeholders with regard to the quality of care and its follow-up and the reduction and resort to hospitalisation, while hospitals remain the main promoters of the reform.[11]
All stakeholders, including health service mangers, policymakers, clinicians, and users' and carers' representatives, supported the goals of social rehabilitation of users and community care, but they were reluctant to reduce the use of hospitals. Clinicians and hospital managers were averse to changes in the treatment processes, particularly in relation to hospital admissions and mechanisms for greater integration of patient care.[1]
Although the reform blueprint clearly stated that the “reform cannot be organised exclusively from the hospitals”, they are nonetheless the main providers of mental healthcare. The hospitals define their plans for networking, select their community partners, define the nature of their partnerships, appoint and pay for the network coordinators, and ultimately supply the main source of funding for the networks, including the new mobile teams. Although the reform aims for a balanced integration of hospital and community resources into care delivery networks, this approach to implementation and funding is highly likely to keep the power in the hands of hospitals.[1]
Bibliography
[1] Implementing a Nation-Wide Mental Health Care Reform: An Analysis of Stakeholders' Priorities, Vincent Lorant, Adeline Grard and Pablo Nicaise, 2016, Community Mental Health Journal, https://link.springer.com/article/10.1007%2Fs10597-015-9932-y, accessed 10 August 2019
[2] How does policy learning occur? The case of Belgian mental health care reforms, Sophie Thunus and Frédéric Schoenaers, University of Liège, 11 May 2017, https://www.tandfonline.com/doi/full/10.1080/14494035.2017.1321221, accessed 13 September 2019
[3] Good Practices in Mental Health and Wellbeing: Mental Health Services in the Community, 2018, Consumers, Health, Agriculture and Food Executive Agency (Chafea), the European Commission, https://ec.europa.eu/health/sites/health/files/mental_health/docs/2018_goodpractices_en.pdf, accessed 5 August 2019
[4] Mental Health Declaration for Europe - Facing the Challenges, Building Solutions, WHO European Ministerial Conference on Mental Health, Helsinki, Finland, 12-15 January 2005, http://www.euro.who.int/__data/assets/pdf_file/0008/88595/E85445.pdf, accessed 12 August 2019
[5] How healthy is mental health care in Belgium? The facts behind the myths, 1 July 2013, Itinera, https://www.itinerainstitute.org/en/article/how-healthy-mental-health-care-belgium-facts-behind-myths/, accessed 13 September 2019
[6] The Belgian reform in mental health care: Where are we now? A short overview and state of progress, Bernard Jacob, 2016, Journal of Psychiatry,
https://www.longdom.org/conference-abstracts-files/2378-5756.C1.014-017.pdf, accessed 15 August 2019
[7] Mental health care delivery system reform in Belgium: The challenge of achieving deinstitutionalisation whilst addressing fragmentation of care at the same time, Pablo Nicaise, Vincent Dubois and Vincent Lorant, April 2014, Health Policy Vol 115,
https://www.sciencedirect.com/science/article/abs/pii/S0168851014000542, accessed 9 August 2019
[8] Mental Health Policy and Practice across Europe, Martin Knapp, David McDaid, Elias Mossialos and Graham Thornicroft, 2007, WHO on behalf of the European Observatory on Health Systems and Policies,
http://www.euro.who.int/__data/assets/pdf_file/0007/96451/E89814.pdf, accessed 15 August 2019
[9] Multisectoral Mental Health Networks in Belgium: An example of successful mental health reform through service delivery redesign, Liesbeth Borgermans, Bernard Jacob, Magda Coture and Paul De Bock, 2018, WHO Good Practice Brief,
http://www.euro.who.int/en/health-topics/Health-systems/health-systems-response-to-ncds, accessed 10 August 2019
[10] Belgium: switching to community mental health care, WHO, 12 May 2016,
https://www.who.int/mental_health/evidence/outreach_teams_belgium/en/, WHO, accessed 7 August 2019
[11] Mental Health Action Plan 2013-2020, April 2019, WHO Evidence and Research report, https://www.who.int/mental_health/evidence/outreach_teams_belgium/en/, accessed 14 August 2019
[12] Joint Action on Mental Health and Well-being - Towards community-based and socially inclusive mental health care, J.M. Caldas Almeida, Pedro Mateus and Gina Tomé, 2017, EU Assessment Report,
https://ec.europa.eu/health/sites/health/files/mental_health/docs/2017_towardsmhcare_en.pdf, accessed 15 August 2019
[13] La réforme des soins en santé mentale en Belgique: exposé d'un modèle, Bernard Jacob, Donatien Macquet and Stéphanie Natalis, November 2016, L'information Psychiatrique, Volume 92/9, p. 731-745,
https://www.cairn.info/revue-l-information-psychiatrique-2016-9-page-731.htm, accessed 15 August 2019
[14] Guide vers de meilleurs soins de santé mentale par la réalisation de circuits et de réseaux de soins, 26 April 2010, Belgian Ministry for Health
, accessed 14 August 2019
[15] Mental Health Care, For a Healthy Belgium, 24 April 2019, https://www.healthybelgium.be/en/health-system-performance-assessment/specific-domains/mental-health, accessed 7 August 2019
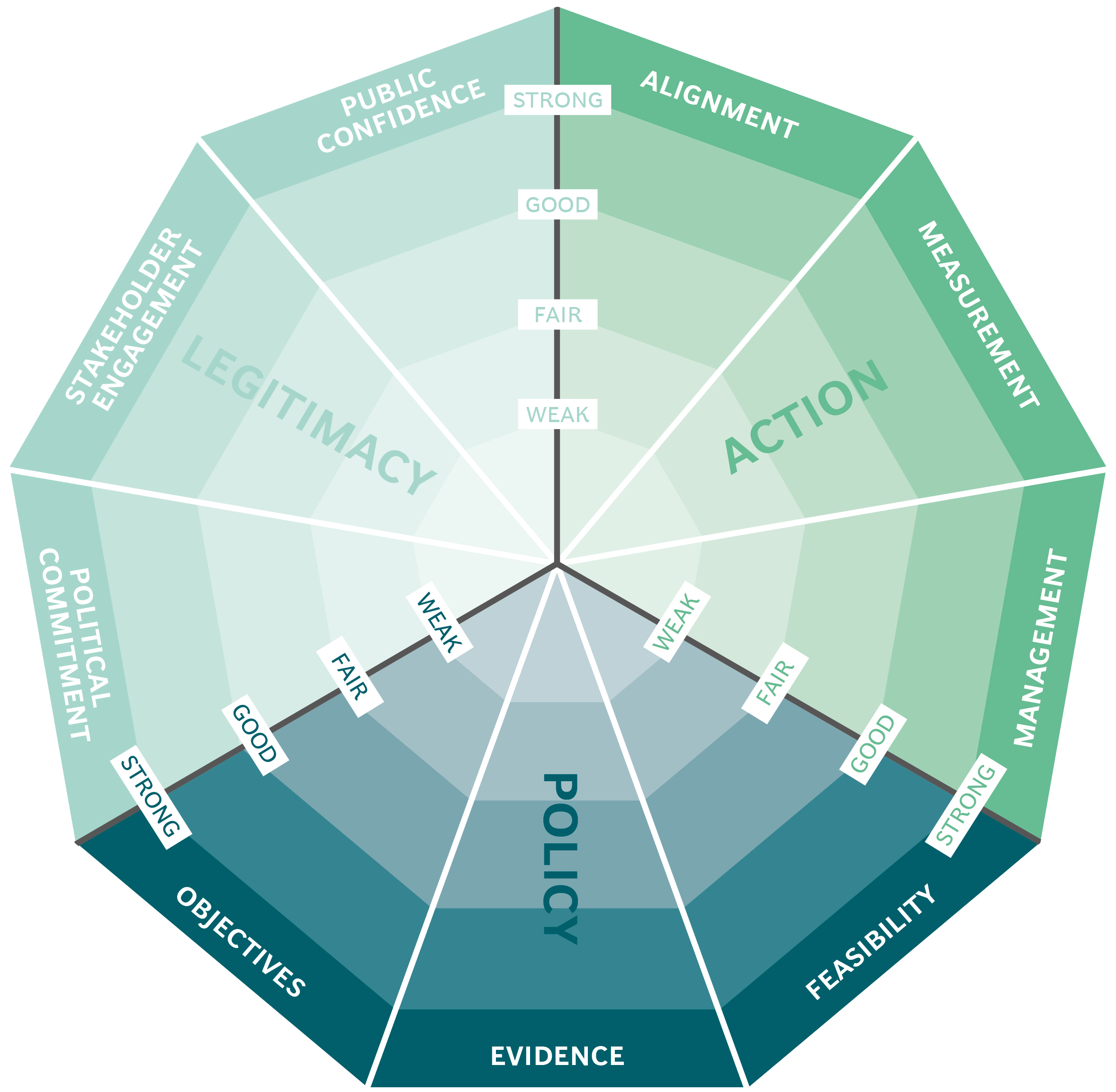
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
