
Peer Respites in the US
The initiative
One of the community-based approaches to tackling mental health is already present in the US. Ever since the numerous legislative efforts to deinstitutionalise mental health and substance abuse systems from the 1960s onwards, there has been a growth of centres that have come to be known as Peer Respites. Currently, there are 22 such respites across the country, all of which have been founded by community grassroots organisations.[6]
These Peer Respites are voluntary, short-term, overnight programmes that provide community-based, non-clinical crisis support to people who are experiencing or are at risk of a psychiatric crisis. The Peer Respite centres operate 24 hours per day in a homelike environment and are staffed by people who have experienced challenges to their mental health. The idea is that individuals suffering from mental health problems can check themselves in and stay for a short period of time (between 3 and 90 days, depending on individual centres) and receive peer support and guidance.[6]
Many of the respite centres in the US have been founded since 2008, although some of the centres are older and were founded as branches of community peer support initiatives.[6] The Hacienda of Hope in Long Beach, California has elements of both characteristics. It was founded as a Peer Respite in 2014, but its origins go back much further, being part of the “Project Return Peer Support Network”, which has a 35-year history of furthering peer support systems.[7] Whilst many of the current centres have their origins in previous peer support initiatives and take guidance from umbrella organisations such as the NEC, the respite centres themselves are wholly peer-operated and peer-run.
Peer Respites are intended to operate as a mechanism for “crisis diversion” for mental health sufferers. Where individuals suffering from mental health difficulties would usually follow a path leading from “psychological stressors” to psychiatric crisis, ultimately followed by costly and often unhelpful psychiatric emergency services, Peer Respites try to act as an intervention in the stages preceding the use of emergency services.[6]
Peer Respites provide a safe place for people to go during a mental health crisis.[8] They are staffed and operated by peers, that is, people who have experienced mental health problems themselves and have also received professional training in providing crisis support.[5] The aim of Peer Respites goes beyond improving health outcomes and reducing the financial burden on emergency services. They are also seeking to alter the framework of how mental healthcare is provided to those with mental health difficulties and to create an alternative to the traditional and often impersonal model of mental healthcare administration.[6]
The challenge
There is a growing concern in many countries, including the US, about the escalation of mental health issues. For example, approximately 1 in 5 adults in the US (46.6 million) experiences a mental health condition in a given year; suicide is the 10th leading cause of death in the US, and the 2nd leading cause of death for people aged 10-34, and more than 90% of people who die by suicide show symptoms of a mental health condition; and the financial burden of serious mental health illness in the US amounts to approximately $193 billion in lost earnings per year [1].
Mental Health America (MHA), a leading community-based non-profit dedicated to addressing the needs of those living with mental health conditions, has criticised the current system of administering treatment to those experiencing mental health conditions as one of the principal obstacles to individuals receiving appropriate care. MHA highlights the fact that many regions of the US operate with a rigid “medical model” of care, whereby people seek health treatment only when they feel objectively sick, as opposed to a subjective feeling of mental unease. As regards mental health, it is more a feeling of wellness rather than “visible” illness that is the concern of the patient, which is not immediately compatible with the prevailing medical model. This creates difficulty for individuals in the initial stages of mental health crises, because it creates uncertainty in identifying when someone should be seeking mental healthcare.[2]
At the same time, there has been a growing desire among US policymakers to move away from a model of mental healthcare based on psychiatric institutions.[3] This desire is also shared by stakeholders who work in or receive mental health treatment. This contributes to a growing demand for community-based alternatives for providing mental health support. But according to a 2005 report by the National Empowerment Center (NEC) - an advocacy organisation that promotes an empowerment-based recovery model of mental health - frontline healthcare workers often feel isolated and unable to air their views.[4]
These factors have together created a growing consensus that the hierarchical and intrusive nature of America's institutional model of healthcare stigmatises individuals with mental health problems, can hinder processes of social inclusion and recovery, and also places a heavy financial burden on citizens.[5]
The public impact
Due to both the isolated nature of Peer Respites and the often informal way in which they are founded, their relative success or progress has not been easy to measure.[3] Despite that caveat, the initial data does suggest that respites can have a positive influence in reducing individual reliance on inpatient and emergency services and improving the symptoms, social functioning and self-esteem of Peer Respite users. The authors of a 2015 study found that the likelihood of respite users using emergency services was 70 percent lower than for non-respite users. “By reducing the need for inpatient and emergency services for some individuals, peer respites may increase meaningful choices for recovery and decrease the behavioural health system's reliance on costly, coercive, and less person-centred modes of service delivery.”[8]
Furthermore, among those individuals who would tend to call on emergency psychiatric services, a longer stay of up to 14 days within a Peer Respite was associated with fewer hours of emergency services use.[8] Thus, by reducing the need for inpatient and emergency services, there is evidence that Peer Respites serve to reduce overall healthcare costs.[8] The findings of one study suggest that respite users cost USD211 per day on average, compared to USD665 per day for those who were hospitalised.[9]
With only 22 centres across 14 states, Peer Respites have a small presence relative to the entire infrastructure of US mental health and substance abuse services. Therefore, while the recorded success of current respite centres is encouraging, more research needs to be carried out to enhance understanding of their functionality.[10]
Stakeholder engagement
The way in which Peer Respites have developed means that there has often been a minimal level of engagement across the entire field of potential stakeholders. While some stakeholders, such as community members and mental health sufferers, have been engaged throughout the development of respite centres, other stakeholders, such as the federal and state governments, have had minimal engagement.
Stakeholders of Peer Respites include federal and state governments, mental health service users, people working in mental health facilities, pharmaceutical companies that manufacture drugs designed to tackle mental health symptoms, and the general public.
Due to their organic formation, each respite has engaged its stakeholders in its own way. Overall, respites remain largely isolated from key mental healthcare stakeholders, such as medical experts and federal or state governments. The Peer Respites are entirely a product of civil society action, founded, staffed and operated by people with psychiatric histories.[6] These centres utilise a network of knowledge and advice from umbrella organisations such as the NEC, Peerrespite.net, and regionally based organisations such as the Project Return Peer Support Network. While these organisations are able to call on an array of experts, their level of involvement from one Peer Respite to the next is inconsistent. As these programmes become more widely known at a state and federal level, it remains to be seen whether they will enjoy more involvement and support from state and federal actors.
Political commitment
State and federal governments have fundamentally failed to make the substantial financial contributions necessary to give Peer Respites nationwide coverage.
However, the federal government has made many attempts over the years to facilitate a transition towards community care and peer support centres. These include:
- The Community Mental Health Act of 1963, which was instituted to provide funding for community mental health centres and promote community-based care as an alternative to hospitalisation
- Reductions in the coverage of Medicaid for acute psychiatric care, such as the denial of financial coverage for inpatient services for persons between the ages of 21 and 65, known as the Institutions for Mental Disease rule, have forced states to use rely more upon community-based services
- Federal disability laws such as the Civil Rights of Institutionalized Persons Act of 1980
- Regulations implementing the US Supreme Court's decision in Olmstead v. L.C., 527 U.S. 581 (1999), which was based on the American with Disabilities Act and instructed states to use community alternatives to inpatient care, where they were reasonable and appropriate.[11]
More recently, the 2002 New Freedom Commission's report indicated that the nationwide health focus is primarily based on those with severe disabilities and general illness, rather than wellness. As a consequence, measures “have failed to serve the great majority of individuals who suffer significant but not catastrophic disorders”.[2]
Despite this, the federal government has yet to introduce a policy or initiative to expand Peer Respites, currently numbering only 22. The lack of a consistent model of government funding, along with the sporadic development of Peer Respites, has led several key stakeholders and advocacy groups to describe it as a “peer-run crisis respite movement”, rather than as a coherent programme or government policy. [9]
These initiatives have promoted a move towards greater community-level care. However, there is a need for a policy framework and greater funding, within which programmes could develop services to meet local needs. The deinstitutionalisation movement that began in the 1960s has certainly resulted in changes to mental health and substance abuse treatment, thanks to its promotion and development of community-based care. However, MHA argues that these care centres remain on the whole siloed, fragmented and inadequate.[2] As a consequence, access to effective, community-based services and support is, for many people, extremely limited.
Public confidence
While there is currently minimal evidence demonstrating the degree of public confidence in Peer Respites, there is some evidence of support - among mental health experts and the public - for the role that peer-to-peer community organisations play in tackling mental health issues.
The NEC, one of the NGOs championing the claims of Peer Respites, developed an approach to mental health called Personal Assistance in Community Existence (PACE). This approach is based on the premise that people can recover fully from the most severe mental illness on an Empowerment Model of Recovery and Prevention.[12] A national survey into PACE conducted in 2005 found that the PACE programme had changed respondents' attitudes towards mental health treatment [4]. The report indicated that a majority of respondents had not previously thought of mental health treatment as having community-based solutions, and that they would not be averse to seeing it administered in this way.
Clarity of objectives
Peer Respites have two primary objectives: to challenge the way mental healthcare is administered in the US; and to provide mental health service users with a safe space in which to support each other. They empower individuals to take more prominent roles within their community in giving early access care to individuals suffering from mental health issues.[6]
Peerrespite.net is a website governed by a panel of experts with experience in Peer Respites and other peer-run organisations in the US and is tasked with offering information and guidance about them. Its view is that: “Peer Respites were designed as psychiatric hospital diversion programmes to support individuals experiencing or at risk of a psychiatric crisis. The premise behind peer respites is that psychiatric emergency services can be avoided if less coercive or intrusive supports are available in the community.”[6]
As Peer Respites have sprung from a grassroots movement rather than a government policy, the experts and key stakeholders involved are in full agreement about their overarching objectives. For example, the Monadnock Peer Support Centre in New Hampshire states its objective as: “to establish a culture in which our members and participants feel more empowered and less dependent on the mental health system”.[13] This objective is echoed by other respites, for example, the Monarch House Peer Run Respite in Wisconsin, which states that its objective is to “provide a supportive, home-like environment where people can explore, discover, and direct their path to healing and wholeness”.[14] Both of these respites, and others like them, offer a more welcoming culture than the institutionalised emergency service system.
Strength of evidence
Before the growth of Peer Respites - from 2008 onwards - there was a strong base of evidence in favour of peer-to-peer services for individuals with mental health-related conditions.[15] This is often attributed to the interpersonal nature of peer-to-peer care, where those involved with administering care or treatment are more sympathetic to the difficulties facing service users. [15] This outlook on healthcare, and the relationship between the individuals involved, runs counter to the assumptions of the predominant medical model. There is a lack of recent evidence on the performance of Peer Respites, which is likely related to both the small number of recognised Peer Respites in the US and the degree of inconsistency in their operating models.
One randomised controlled trial in 2008 documented self-rated mental health functioning and satisfaction for respite users compared to users of a locked, inpatient psychiatric facility (LIPF). The study found that the Peer Respite had a positive influence on its users' mental health: they “experienced significantly greater improvement on interviewer‐rated and self‐reported psychopathology than did participants in the LIPF condition [and their] service satisfaction was dramatically higher”.[16] Thus, there is a recognition that more comprehensive research needs to be carried out across the spectrum of currently operating Respite Centres to enhance understanding of their functionality.[10]
Feasibility
Despite the structural obstacles to reorganising the way mental health treatment is thought about and administered, there is strong recent evidence that Peer Respites have proved successful and financially feasible.[17] An investigation run by the Substance Abuse and Mental Health Services Administration (SAMHSA) found that, overall, respite centres offered a less expensive alternative to hospitalisation. They were generally run at a 20 to 30 percent lower cost.[18] The presence of these respites in a community also has the benefit of reducing overall health costs, as 70 percent of respite users were less likely than other mental health sufferers to use inpatient or emergency services.[18] This view was supported by findings that average psychiatric hospital costs were USD1,057 for respite users compared to USD3,187 for LIPF users.[18]
Due to the complexity of the US healthcare system, and because Peer Respites are grassroots organisations, the financial model of support for these centres casts some doubt on their feasibility. The average income distribution of respite funding in percentage terms is as follows: state (46), county (35), Medicaid-managed care (7), federal (3), and other (9).[19] The majority of state funding comes from grants given by the Department of Mental Health and the remaining funds come from local sources.[9] There is a significant dependency on other contributors for funding and the capability of local communities to support Peer Respites has a strong impact on the feasibility of these initiatives. Also, there are significant regional differences in the feasibility of running respites, due to variations in running costs, property ownership, rental fees, and salaries.[17]
Management
Since the deinstitutionalisation movement began in the 1960s, an evolving federal-state partnership promoting community-based care has remained siloed and isolated. This impression was supported by congressional hearings in 2015 and 2016, which concluded that the government mental health and substance abuse systems that serve people affected by mental health issues are severely fragmented.[2]
As a result, the development of Peer Respites has been sporadic and is reliant on grassroots groups, advocacy groups, and NGOs for financial support and guidance. Many respites come under the umbrella of larger not-for-profit organisations or NGOs, such as the NEC.[20] These organisations act as advocates for peer-based mental health support, seeking to share and further best practice among the Peer Respite community. In regard to funding, many respites turn to SAMHSA, the federal organisation responsible for providing leadership, resources and funding for “efforts to enhance the mental health of the nation”, in order to apply for grants.[21]
As stated in Feasibility above, the management and implementation of Peer Respites has varied from place to place. For example, the Georgia Peer Support and Wellness Center allows for a maximum of 3 guests to stay up to 7 days, whereas the New Beginnings Center in West Virginia allows a maximum of 8 guests to stay for up to 90 days. While these differences help each respite to develop its distinct organisational culture and healing environment, they can lead to complications in measuring respites' applicability and effectiveness.
Measurement
Because current Peer Respites are created informally and without governmental direction, they can be isolated from one another and have subtle differences in their structure and operation. For example, some respites require potential users to have full-time accommodation elsewhere whereas others do not, and respites vary in the maximum stay they offer their users (see Management above). These differences make measuring the implementation of Peer Respites more difficult.
However, there is consensus between Peer Respite stakeholders that in order for the programme to gain favour with policymakers, and to ensure that best practice is disseminated, they must be able to track their own progress.[9] Several organisations, such as peerrespite.net and the NEC, are also involved in assessing and circulating this feedback among relevant stakeholders and prospective respite centres in order to track progress more accurately.[6][20]
Alignment
One of the reasons that Peer Respites have failed to gain ground in the US is that their potential stakeholders are pulling in different directions. As detailed above (see The Challenge), the current model of healthcare provision places an emphasis on the treatment of mental illnesses through pharmaceutical prescription drugs.[2] Indeed, the drug lobby in the US has been extremely successful in promoting some of its solutions for an array of mental health concerns over the past 30 years.[2] This may lead some lobbyists and politicians to favour hierarchical medical care, and it impedes the adoption of peer support mechanisms that are advocated by many mental health workers, mental health users, and policymakers.
Consequently, as of 2016, there were only 22 Peer Respites, in just 14 of the US's 50 states. This low number relative to the size of the nation and the urgency of the country's mental health issues indicates the difficulties of creating new Peer Respites within the US mental healthcare system.
Bibliography
[1] Mental Health By The Numbers, National Alliance on Mental Illness, https://www.nami.org/learn-more/mental-health-by-the-numbers, Accessed 4 September 2019
[2] Position Statement 14: The Federal Government's Responsibilities for Mental Health Services, 9 September 2016, Mental Health America, https://www.mentalhealthamerica.net/positions/federal-role, Accessed 15 August 2019
[3] Peer Respites: A Research and Practice Agenda, Laysha Ostrow and Bevin Croft, 1 June 2015, Human Services Research Institute, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4475343/, Accessed 8 August 2019
[4] How the PACE Program Builds a Recovery-Transformed System: Results from a National Survey, J.H. Zahniser, L. Ahern and D. Fisher, 2005, Psychiatric Rehabilitation Journal, 29(2), 142-145,
https://psycnet.apa.org/record/2005-13514-011, Accessed 15 August 2019
[5] Peer Respite Crisis Respites: Research & Practice Initiatives in the United States, Laysha Ostrow, March 13 2014, Lived Experience Research Network, https://www.cibhs.org/sites/main/files/file-attachments/thurs_215_edgeab_ostrow.pdf, Accessed 8 August 2019
[6] Peer Respites: Action and Evaluation, Live & Learn, Inc.,
https://www.peerrespite.net/, Accessed 8 August 2019
[7] History, Project Return Peer Support Network,
http://prpsn.org/about/history/, Accessed 15 August 2019
[8] Impact of the 2nd story peer respite program on use of inpatient and emergency services, B. Croft and N. Isvan, June 2015, Human Services Research Institute, https://www.ncbi.nlm.nih.gov/pubmed/25726982, Accessed 8 August 2019
[9] A Case Study of the Peer-Run Crisis Respite Organizing Process in Massachusetts, Laysha Ostrow, Spring 2010, Heller School for Social Policy and Management,
https://www.ncmhr.org/downloads/Ostrow_Groundhogs-case-study.pdf, Accessed 15 August 2019
[10] Leadership and Characteristics of Nonprofit Mental Health Peer-Run Organizations Nationwide, Laysha Ostrow and Stephania L. Hayes, February 2015, Psychiatry Online, https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201400080, Accessed 15 August 2019
[11] Civil Commitment and the Mental Health Care Continuum: Historical Trends and Principles for Law and Practice, 2019, SAMHSA, https://www.samhsa.gov/sites/default/files/civil-commitment-continuum-of-care_041919_508.pdf, Accessed 15 August 2019
[12] Recovery at your own PACE (Personal Assistance in Community Existence), Ahern L., Fisher D., 2001, Journal of Psychosocial Nursing Mental Health Services,
https://www.ncbi.nlm.nih.gov/pubmed/11324174, Accessed 15 August 2019
[13] Who We Are, Monadnock Peer Support
https://www.monadnockpsa.org/about, Accessed 15 August 2019
[14] Monarch House Peer Run Respite, Wisconsin, Milkweed Alliance, https://www.milkweedalliance.org/monarch-house, Accessed 15 August 2019
[15] Peer Support Services for Individuals With Serious Mental Illnesses: Assessing the Evidence, Matthew Chinman et al, 2014, Psychiatric Services,
https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201300244, Accessed 15 August 2019
[16] A randomized trial of a mental health consumer-managed alternative to civil commitment for acute psychiatric crisis, T.K. Greenfield, B.C. Stoneking, K. Humphreys, E. Sundby and J. Bond, 2008, American Journal of Community Psychology,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2782949/, Accessed 15 August 2019
[17] "So You Want To Start a Peer-Run Respite?" Daniel B. Fisher, Rigel Flaherty, Daniel Hazen and Steve Miccio, October 2011, YouTube Webinar, https://www.youtube.com/watch?v=n7b7A6NDmbk, Accessed 15 August 2019
[18] Peer-run Respites: An Effective Crisis Alternative, Daniel B. Fisher, Bevin Croft, Val Neff, Camille Dennis, Jayme Lynch and RoslindHayes, SAMHSA, https://www.nasmhpd.org/sites/default/files/Peer%20Run%20Respite%20slides.revised.pdf,Accessed 15 August 2019
[19] Results from the 2016 Peer Respite Essential Features Survey, Laysha Ostrow and Bevin Croft, peerrespite.net, https://www.nasmhpd.org/sites/default/files/PREF%2BReport%2B050516_FINAL.pdf, Accessed 15 August 2019
[20] Programs and Services, National Empowerment Center,
https://power2u.org/what/, Accessed 15 August 2019
[21] Who Are We, SAMHSA
https://www.samhsa.gov/about-us/who-we-are, Accessed 15 August 2019
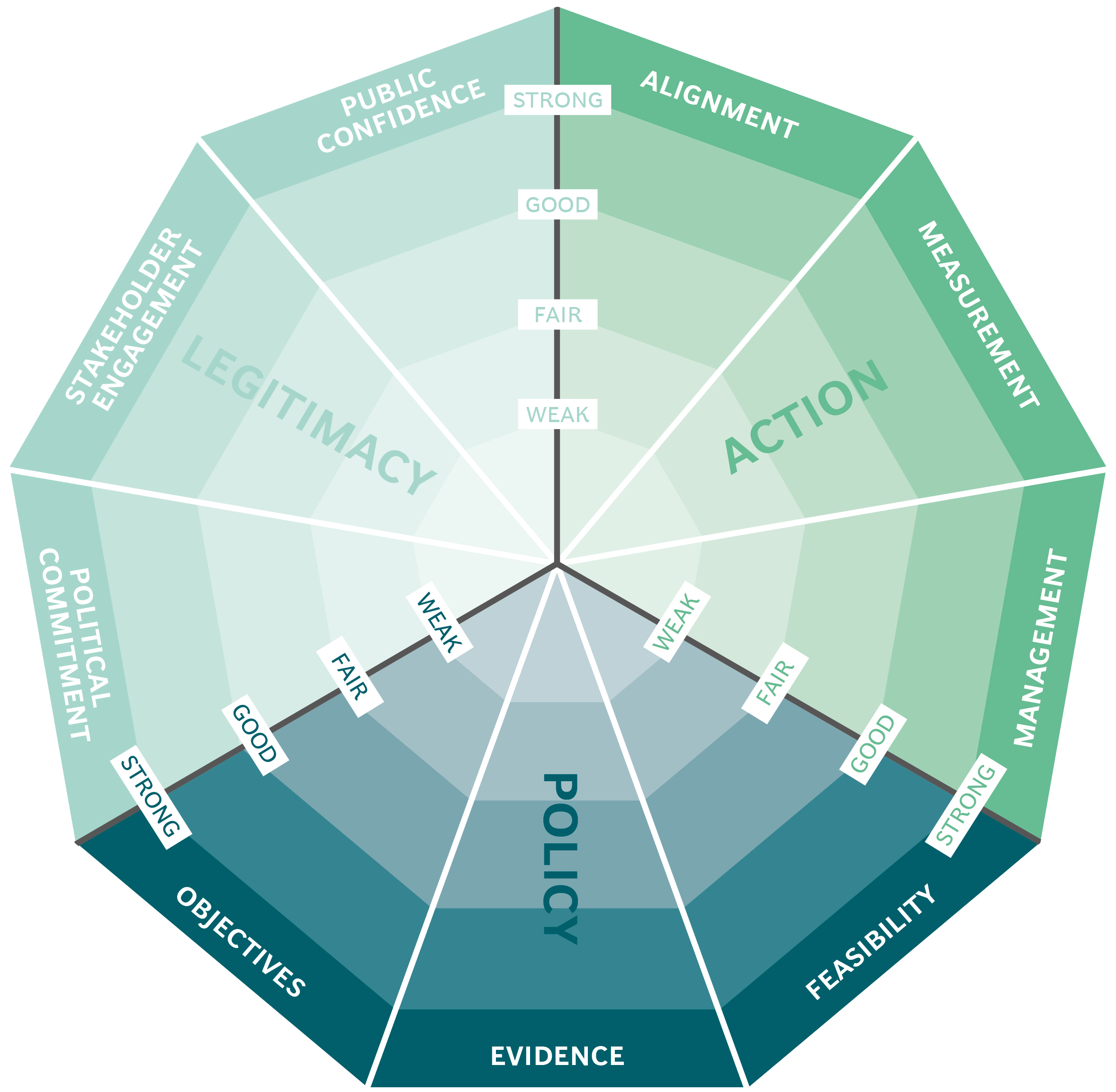
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
