
Career Coaching at the Central Baptist Hospital in the United States
Much like the rest of the US population, the nursing sector has found itself with a significant number of ageing workers. As the “baby boomers” have started to reach the retirement age of between 65 and 67, the proportion of ageing workers in the workforce has been increasing. Central Baptist Hospital in the state of Kentucky in the US recognised that this trend, coupled with insufficient numbers of nursing graduates, would require them to develop a strategy for retaining older nurses.
In 2008, under the management of Karen Hill, the Career Coaching programme was launched at the hospital, with the aim of retaining senior nurses through flexible strategies that reflected their needs. The programme was designed to help maximise nurses' working experience, as well as provide managers with the tools to help nurses fulfil their potential. The Career Coaching programme successfully helped reduce Central Baptist's nursing vacancy rate, increase nurses' job satisfaction, and facilitate nurses' professional development.
The initiative
Central Baptist Hospital is committed to delivering high standards of healthcare and professional leadership. Their vision statement outlines their aim to be “an innovator in the delivery of health services, anticipating and responding to a changing healthcare environment through collaborative models that are outcome driven, financially responsible, and supportive of their mission”.[5]
This ethos underpinned the Career Coaching programme launched in 2008 as part of CEO and Nursing Officer Karen Hill's research project, The Nursing Leadership Succession Map: A Pilot Study. The programme's main objectives were to retain nursing expertise by offering flexible working options to nurses. Retired nurse Carol Komara was recruited by Hill to be the career coach, whose role was to “identify leadership competencies, educational needs, and to develop plans to meet the career goals of the nurse”.[6] She facilitated “individuals with a career plan within an organisation's structure, which is mutually beneficial and supportive to both the individual advancing on a planned career path as well as the organisation's goal for leadership development and succession planning.”[6]
Key components of the programme were providing opportunities for nurses to re-career and offering flexible working hours. Re-careering for nurses involved “transitioning to different nursing roles or schedules or continuing their education and moving into other healthcare practice areas”, while flexible working hours were made possible, such as “part-time, seasonal positions with healthcare benefits to match those of full-time employees”, moving “from full-time to part-time while remaining in the same position/level”, or transferring “to a job with reduced patient care responsibilities”.
The Career Coaching programme was conducted with an initial meeting between Carol Komara and individual nurses participating in the programme, to draw up an action plan and review the nurses' career goals. A month later, a follow-up meeting was used to review data, discuss the action plan further, and update the employee's documentation form, taking into account what resources were needed to achieve the action plan, for example financial support or a career shadowing opportunity. Following this, the nurse and career coach would communicate to evaluate progress and discuss any further plans for career development. Komara would also inform management of any relevant information regarding the future career path of individual nurses.[6]
The challenge
In recent years, the United States healthcare sector has found itself in an increasingly difficult situation: the demand for healthcare services is increasing, while the supply of healthcare staff is facing shortages, notably in the case of nursing.[15]
This increased demand for healthcare services can be attributed not only to changing patient demographics, with increasing numbers of older citizens, but also to the fact that, as of 2005, one in two Americans suffered from a chronic disease.[10]
The decrease in the number of nurses can be explained by an ageing workforce, a smaller pool of qualified nursing graduates, and unfavourable working conditions.[15] Understanding the scale of the latter problem was of primary importance to Central Baptist. As the “baby boomers” - individuals born between 1946 and 1964 - approach retirement, the number of older workers participating in the workforce has increased significantly: “for people aged 55 to 64, the labour force participation rate increased modestly from 57.2 percent in 1995 to 59.1 percent in 2000. It subsequently rose at a much faster pace, to 65.3 percent in the first half of 2009.”[1] This can be attributed to two factors: “the first is strictly demographic - in particular, the passage of the outsized baby boom generation … into older age. The second is changes in work-related behaviours - a rising share of older adults are working or looking for work and, conversely, an increasing share of youth are staying in school and not looking for work.”[1]
Furthermore, a decline in the number of nursing school graduates was caused by a lack of faculty expertise and resources in nursing schools rather than a shortage of applicants.[10] Although Central Baptist Hospital was aware of such trends they “felt insulated in the beginning, because [they] had a younger workforce and many schools in the area”.[5] However, by 2008 Central Baptist had recognised that the trend was also affecting their hospital. The nature of nursing work is physically and mentally demanding, which leads to some nurses retiring earlier than the national retirement age of between 65 and 67.[12]
At Central Baptist, almost half of the workforce was over 49, and the average retirement age was 64 hospital-wide in 2008.[5] However, due to the demanding nature of the work, many nurses began “to scale back their hours or retire at age 55”. The average age of registered nurses (RNs) had been steadily rising: in 2008, the average age of an RN was 47, up from 40.3 years in 1980. In 2000, 33 percent of RNs were over 50; however, by 2008 this figure was up to 45 percent.
Central Baptist, appreciating the challenge, had to develop a “flexible work policy” across the organisation to combat the potential loss of knowledge and expertise that the organisation would experience with the older workers' retirement.[5] The hospital was aware that “replacing experienced workers is costly and research demonstrates that losing nursing experience can have a negative impact on patient quality of care, safety, and satisfaction, as well as employee engagement and organisational performance.”
The public impact
The Career Coaching programme proved successful in the areas of staff retention, employee engagement and re-careering in Kentucky. Retention of staff improved in Central Baptist, with the rate of staff turnover being below the national average for healthcare. Moreover, the “vacancy rate” (the average number of vacant full-time equivalent positions divided by the average number of budgeted full-time equivalent positions) was 1.8 percent hospital-wide as of 2011 and has been below 3 percent since 2008.” In 2007, the vacancy rate of RNs had been 5 percent in hospitals in Central Baptist's Area Development District - the Bluegrass region - and 6 percent on average in hospitals statewide.
RNs aged 45 and over were polled on their job satisfaction and results showed an improvement in workplace satisfaction from 65 percent in 2006 to 88 percent in 2010. Furthermore, of those surveyed 90 percent agreed with the statement “I feel I am a part of a team” in 2010, whereas the figure had been at 53 percent in 2006. Thanks to Career Coaching, “nurses have returned to school; one received a prestigious award; another had an article published in a medical journal; several applied for advanced positions; and one joined her local Chamber of Commerce to gain leadership experience in her community”.
One part of the programme was to make the necessary resources available to nurses to develop professionally and, as a result, “three employees from the programme have been awarded Nursing Incentive Scholarship Funds from the Kentucky Board of Nursing to assist with educational cost”.[6] Working to remove other barriers to career advancement, such as lack of access to information and further education, prompted the hospital to host an education fair on site, having discovered “there was confusion about the current educational programmes and opportunities for nurses to advance”.[6] Komara stated that the fair “was an impetus for many of the nurses to think more seriously about future education and advancement and begin planning for their future careers in nursing”.[6]
Lastly, as the programme had proved to be valuable in many ways, Central Baptist planned to expand it in order to:
“Involve additional participants from the nursing staff”
Offer “a variety of positions to retired nurses”
Consider “creating additional, temporary positions for those workers who are delaying retirement”
Offer “additional resources to support older, experienced nurses, based on feedback from the coach and the Senior Nurse Advisory Council”
Work “with managers to help develop their coaching skills”.
Written by Ella Jordan
This case study is part of a series of international policies that focus on easing the transition to retirement and later life. The case studies and the accompanying report were produced for the Calouste Gulbenkian Foundation (UK Branch).
Stakeholder engagement
The key stakeholders in the Career Coaching programme were well-engaged and showed solid support. The programme was developed by Central Baptist's administrators who believed that they had to “focus on listening to employees - especially older employees - before they implement new approaches to work”. Taking into account workers' ideas, the hospital developed its strategy to:
Retain experienced workers by offering flexible work schedules
Enhance employee satisfaction and engagement by training managers to approach employee issues with flexibility
Expand succession planning of mid-career and late-career staff through mentoring, training and tuition reimbursement.
Career Coaching was run by Karen Hill, who was committed to the programme and to researching the best ways to maximise nurses' potential for their own personal benefit as well as that of the hospital. She said that the hospital's “philosophy of flexibility changes as we respond to the changing workforce. We are cautious to balance our response to meeting older workers' needs with what's right for other generations as an employer of choice.” Carol Komara, who managed the programme, had recently retired from a nursing career that had “included working in labour and delivery, establishing her own prenatal education practice, and serving in management and then nursing education roles”.[14]
Political commitment
Political commitment to the programme was good, as the majority of actors showed solid support. Central Baptist Hospital is a member of Baptist Health, a private, not-for-profit healthcare network serving Kentucky. Both at a hospital and programme level, top-level management was committed to retaining older workers for the workers' benefits as well as the hospital's. Central Baptist “believes in giving its employees opportunities to ‘recreate themselves', and in redeveloping roles so that individuals' potential can be maximised. Central Baptist also works to promote constructive relationships at the workplace by encouraging positive, supportive interactions between employees through a caring framework.”[5] Similarly, “the administrators of CBH believe they must focus on listening to employees - especially older employees - before they implement new approaches to work.”
Karen Hill was committed to finding ways to help nurses thrive professionally, as well as providing excellent standard of care in the hospital. She said: “An approach for flexibility has to be a mindset from the top. It has to be an organisational priority, not just something employees want. We have worked really hard to raise the consciousness of our leaders and were successful in incorporating flexibility into the organisation's strategic plan.”
The hospital was also clearly dedicated to achieving excellence and supporting staff success. This dedication manifested in its achievement of attaining Magnet Recognition status in 2005. The recognition is awarded by the American Nurses Credentialing Center, a subsidiary of the American Nurses Association as a marker of nursing excellence given to only 4% of health care organisations in the United States. Its objective is to “promote quality in a setting that supports professional practice; to identify excellence in the delivery of nursing services to patients; and to disseminate best practices in nursing services.” To be eligible, hospitals have to collect data at the unit level and “benchmark that data against national, state or regional databases.”[16]
After the Career Coaching programme, the hospital was redesignated with Magnet status in 2010 and 2015, being one of only two hospitals in the state to achieve triple-recognition and one of five in the state with the status.[7] In 2015, Hill commented on this award stating how it showed the commitment of the hospital to this: “Our achievement of this credential for an additional four years underscores the foundation of excellence and values that drives our entire staff to strive harder each day to meet the healthcare needs of the people we serve. Less than 140 hospitals in the world have achieved this recognition for a third time."[3]
Public confidence
Public confidence in the programme was good, as the public broadly trusted Central Baptist in particular and programmes that aimed to improve the quality of patient care in general. In recent years across the US, pressure on hospitals to participate in quality improvement activities has increased, with the aim of improving patient outcomes. Thus, a focus on improving and measuring hospital performance creates the potential for patients to benefit from increased quality of care as well as making it possible to compare hospitals regionally and nationwide using standardised measures. Central Baptist was dedicated to providing excellent standards of patient care, and it recognised that experienced nurses were integral to this.
In 2010, a National Institute of Health study found that “better hospital nurse work environments have been linked empirically with higher job satisfaction and lower nurse burnout, and to lower risk-adjusted mortality and failure-to-rescue rates. [Their] new findings supply additional evidence suggesting that improving nurse work environments in hospitals could result in improved patient outcomes, including better patient experiences.”[9] One measure of patient satisfaction was the Centers for Medicare and Medicaid Services' voluntary “Hospital Quality Initiative (HQI), under which hospitals report a core set of quality measures for display on a public Web site”. Research conducted in 2008 by the Center for Studying Health System Change noted that “The public nature of the HQI information pressures hospitals not only to participate by reporting, but also to perform well relative to competitors and show improvement”.[6]
It also highlighted the fact that “hospitals often participate in specific quality improvement activities to support staff professional interests.”[16] Therefore, the connection between patient satisfaction, nurses' workplace satisfaction, and nurses' professional opportunities suggests that programmes such as Career Coaching, whose aim was to retain experienced nurses and increase their job satisfaction, would be seen favourably by the public. Although there is no direct evidence of patient's nursing satisfaction rates at Central Baptist before and after Career Coaching, it is likely that patients would have been in support indirectly, to help retain experienced nurses, further their expertise, and provide a better quality of care to patients.[9]
Clarity of objectives
The objectives of the Career Coaching programme were not stated by Central Baptist at the programme's outset, which means that the overall goal of the programme was not as clear as it could have been. The objectives were only later stated in a 2012 case study conducted by The Sloan Center on Aging & Work, which was sponsored by Central Baptist. The objectives were:
“To develop leadership succession and retain organisational talent
“To improve the pathways for knowledge transfer and succession planning by:
Implementing formal coaching and mentoring to encourage knowledge transfer and professional development
Expanding the focus of succession planning to include re-careering of mid-career and late-career staff
“To increase the retention of older experienced nurses by:
Enhancing employee satisfaction and engagement among older, experienced staff
Implementing flexible scheduling options to encourage nurses to delay retirement.”
The small scale of Career Coaching, which was initially available to the nurses in only one unit, allowed Carol Komara to coach 36 nurses for whom “participation in the programme was … optional, informal, and confidential” . During the programme, she learned that there “was confusion about the current educational programs and opportunities for nurses to advance”, so measures were taken to increase nurses' access to information.[6] Financial barriers to education were found to be a problem for some nurses: “therefore reviewing the in-house benefits such as tuition reimbursement and scholarship options have become a major focus”.[6] Thus, while the objectives of the programme were not made explicit to the public, the nurses involved in the programme appear to have benefited from the clarity it brought with regard to desired outcomes.
Strength of evidence
There was a wealth of evidence for Central Baptist to draw on when developing the programme. The hospital was interested in evidence-based practices and committed to providing an excellent standard of nursing. In 2005, “nursing staff and leaders adopted the caring theory of national nursing theorist, Dr Jean Watson, as a framework for [their] healing.”[6] Watson's theory focused on the importance of caring within nursing, “without which nurses may not have been practising professional nursing but instead were functioning as technicians or skilled workers within the dominant framework of medical ‘technocure' science”.[11]
In June 2006, Hill was involved in research into retaining older workers, working as part of the team “that developed the Robert Wood Johnson Foundation (RWJF)-commissioned white paper, Wisdom at Work: The Importance of the Older and Experienced Nurses in the Workplace”.[14] The team recommended investing in “resources to identify, describe, and evaluate best practices for recruiting and retaining older nurses”, as well as “creating expanded roles for experienced nurses and preparing them for those roles; encouraging workplaces that respect and appreciate staff; and equipping managers and supervisors to understand and support an older workforce”.[14] From this paper, Central Baptist took their definition of older worker “as employees age 45 and older”.
Additionally, Central Baptist participated in a study by the Sloan Center on Aging & Work which clarified the needs of their nurses and enabled them to develop a suitable strategy to retain older workers: “they learned that experienced RNs on their staff between the ages of 29 and 65 identified themselves as being in mid-career”. The study considered age through the framework of the Prism of Age, whose “objectives are to encourage employers to challenge generational assumptions and to look beyond chronological age when creating solutions that meet the needs of older workers and businesses”. Central Baptist found elements of the framework such as “socio-emotional age” and relative age of importance to their workplace, the former referring “to developmental changes in psychological development and one's place in the social world” and the latter to “a comparison of an individual's chronological age with a relevant referent group”.
With this information, “they refined their strategy to take ‘phases of careers' and the Prism of Age dimensions into account in the retention solutions they were developing”. For Central Baptist, “focusing on chronological age combined with career stage made more sense … Therefore, all of the scheduling and career flexibility options are available to all employees, regardless of age”.
Feasibility
There were some feasibility challenges that the programme faced at its implementation: funding was made available for only one year, and despite the appointment of the well-qualified Career Coach Carol Komara, the HR department lacked the necessary skills to meet all the needs of older workers.
The Career Coaching programme was made financially feasible by the American Organisation of Nurse Executives, which awarded Karen Hill a single-year grant for her research project “The Nursing Leadership Succession Map: A Pilot Study” in 2008.[13] The annual grant is awarded “to fund nursing leadership research that explores the use of technology to improve safety, enabling nurse leaders and their institutions to make better-informed decisions, and institute positive, measurable changes that could have far-reaching impact on healthcare delivery and patient outcomes across the care continuum.”[13]
In addition to financial feasibility, the required expertise was partly provided for with the appointment of Carol Komara, who was well equipped to respond to nurses' needs. Komara's expertise was essential to enable the HR department to adopt flexible strategies that would be attractive to older workers. HR policies were [56]
Management
The key management figures in the programme were Karen Hill, who oversaw the Career Coaching as part of the her research pilot The Nursing Leadership Succession Map, and Carol Komara. The standard procedure that Komara employed was as follows: firstly, she would meet with nurses and “complete a newly developed competency assessment to identify talents, skills, interests, and educational needs”. One month later, that meeting was followed up on “to review data and begin discussing a plan relative to the employee's career goals”. From that point onwards, Komara would periodically meet “with the employee and/or [email them] to update the plan and determine interventions, outcomes and resources offered (both educational and collegial).” Six months after the first meeting Komara would have “follow-up sessions to evaluate and give feedback to the employee. She [discussed] the progress and [determined] if there [were] further modifications for the career advancement plan.”[6] Using Komara's feedback from the programme, Central Baptist Hospital's HR department was “focused on offering additional resources to support older and experienced nurses”.
Although Hill and Komara both had suitable expertise to run the programme and there was a standard procedure in place, there is no available evidence to show specifically how Hill and Komara co-operated to ensure progress was made regarding the programme's objectives. Despite this, Komara's work as career coach was beneficial to the HR department, who had required knowledge to “understand the steps needed to think strategically, develop a plan, and articulate a case for flexibility and re-careering” as part of the Career Coaching programme.
Measurement
Measurement of the programme was reasonably sound, as there were some metrics in place to measure the programme's success, although they were not complete. While Central Baptist Hospital is generally focused on “assessing employee needs and analysing engagement survey feedback [as] formal components of [its] multiyear ‘Workforce Development Strategic Plan'” the Career Coaching programme was run in a mostly informal way to be flexible to meet employees' needs. However, measuring vacancy rates and nurse turnover provided more substantial evidence of the programme's success. The vacancy rate within the nursing department decreased from 4.2 percent in 2009 to 1.68 percent in 2010, increasing to 1.98 percent in 2011, while the national average for the period was 5.6 percent. Turnover rates for nurses followed a similar pattern, decreasing from 11.11 percent in 2009 to 8.96 percent in 2010 before rising to 10.19 percent in 2011, with the national average being 15.1%.[6]
Carol Komara followed a standard procedure when meeting with and coaching each of the nurses. However, there was no fixed metric in place to consistently measure and contrast different nurses' development.
Alignment
Co-operation between stakeholders on the frontline of the programme was only partially evident. There was a clear alignment between Komara and the HR department, who used her feedback to provide additional resources for older and experienced nurses. Similarly, of the 36 nurses who availed themselves of the programme, 9 pursued advanced degrees and 11 considered school options as a result of Career Coaching.[6]
It was recognised that many managers did not have the necessary skills to lead ageing workers effectively and in such a way as to maximise their potential. Consequently, Komara worked with the HR department to help them develop nurse managers' coaching skills. In addition, there were various initiatives to give nurses access to information about their career options. For example, “an education fair inviting admissions staff from various colleges and universities to share information about degree requirements for roles in the health care industry” was organised for hospital nurses by the HR department, based on Komara's feedback. Training was also provided to give nurses a better understanding of their age-diverse workforce. One such example was ‘Multigenerational Training' which addressed “the differences in generational communication styles and worldviews, and [gave] employees an opportunity to share perceptions around issues of age and generation”.[1]
Bibliography
https://nyam.org/media/filer_public/46/7c/467c2d1d-fa0d-4528-a8fd-347b4bf9dc4d/ase_compendium.pdf
http://assets.pewresearch.org/wp-content/uploads/sites/3/2010/10/americas-changing-workforce.pdf
http://hdl.handle.net/2345/3378
http://docplayer.net/4373509-Kentucky-hospital-association.html
[7] Finding a Magnet Facility, American Nurses Credentialing Center, accessed April 24, 2018.
https://www.nursingworld.org/organizational-programs/magnet/find-a-magnet-facility/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2718727/pdf/nihms124590.pdf
http://www.ijnonline.com/index.php/ijn/article/view/21
http://www.upcolorado.com/excerpts/9780870819797.pdf
[12] Pensions at a Glance: Public Policies Across OECD Countries, OECD, 2007, OECD Publishing
[13] Small Grant Past Recipients, American Organisation of Nurse Executives, April 2018, www.aone.org
http://www.aone.org/aone-foundation/research/smallgrant-past.shtml
[14] ‘The go-to nurses' Finding Ways to Keep Long-time RNs, Susan Trossman, February 2011, The American Nurse
http://journals.sagepub.com/doi/pdf/10.1177/1527154406293968
http://www.hschange.org/CONTENT/972/972.pdf
https://www.rwjf.org/content/dam/farm/reports/program_results_reports/2010/rwjf65925
https://www.rwjf.org/content/dam/farm/reports/reports/2006/rwjf13773
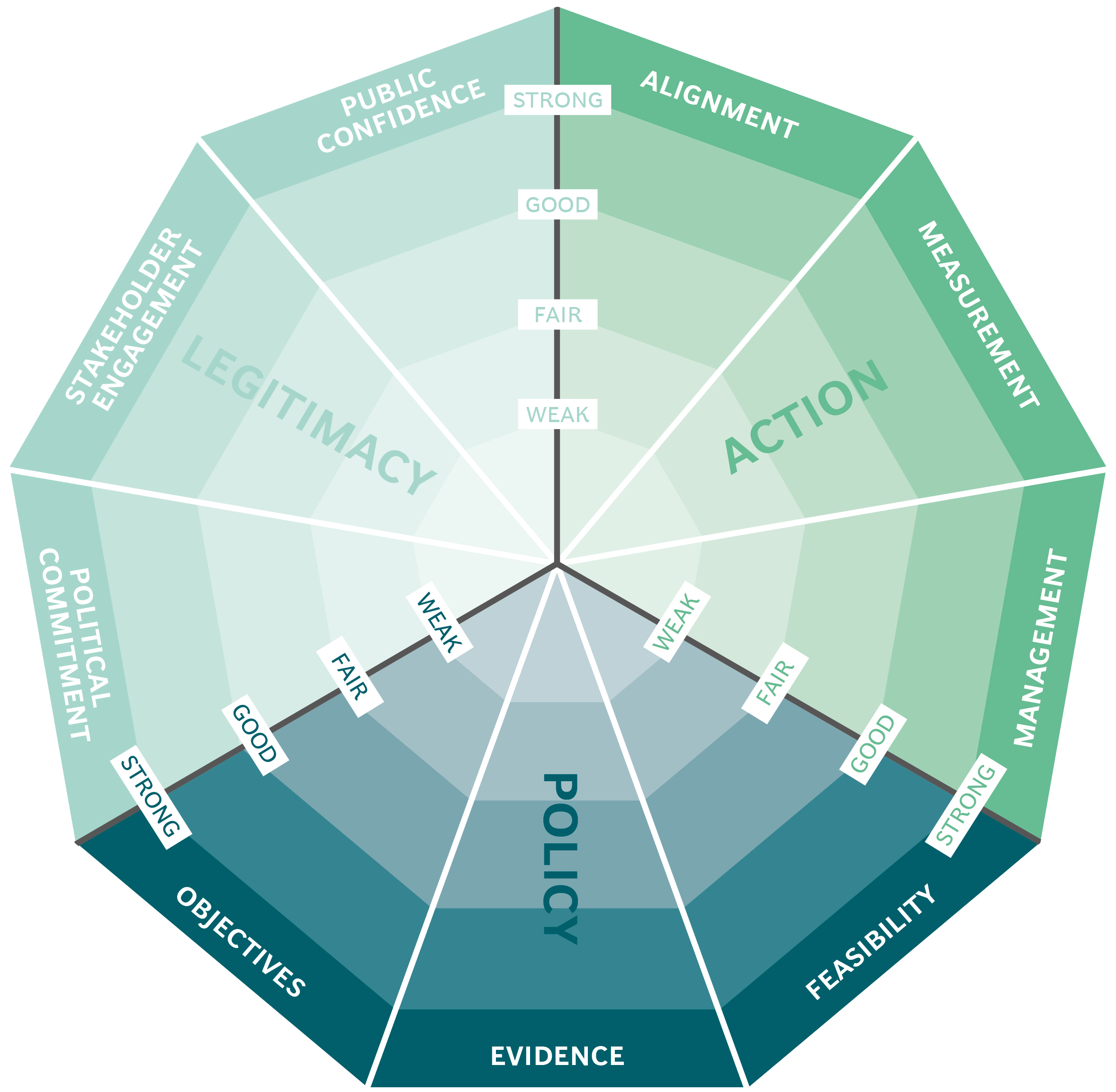
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Mexico City's ProAire programme

BANSEFI: promoting financial inclusion throughout Mexico

Formalising the appointment and compensation of Chile’s senior civil servants

Rainfall insurance in India
